Reglan dosages: 10 mg
Reglan packs: 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Reglan 10 mg purchase on-line
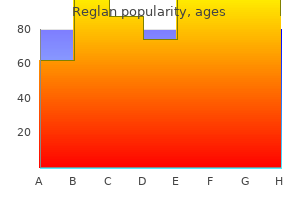
Treatment ought to address several primary issues: (1) removal of air 7 day gastritis diet generic 10 mg reglan, (2) preventing further air accumulation gastritis symptoms and causes quality reglan 10 mg, (3) healing the harm that triggered the initial accumulation, (4) promoting lung reexpansion, and (5) stopping or limiting reoccurrences. With no intervention, a small pneumothorax will resolve over a interval of days to weeks. Supplemental oxygen will velocity the method of lung reexpansion by rising the speed of pleural air absorption. In particular, no vital distinction has been found between simple aspiration and tube drainage with regard to the immediate success fee, early failure fee, duration of hospitalization, and 1-year success and pleurodesis. Frequently, this is followed by diagnostic or therapeutic visual inspection of the lung and pleural area by fiberoptic thoracoscopy. Surgery could additionally be beneficial for a first pneumothorax in the following situations: life-threatening pressure pneumothorax, massive air leaks with incomplete reexpansion, an air leak persisting 4 days after a second tube has been positioned, associated hemothorax with complications, identifiable bullous illness, or failure of straightforward reexpansion in sufferers with cystic fibrosis. In patients with traumatic causes, the urgency and sort of treatment rely totally on the steadiness of the patient; a hypotensive affected person with a rigidity pneumothorax requires instant decompression with a chest tube or needle thoracostomy, whereas a patient with normal vital signs and a small pneumothorax could also be observed initially. Emergency needle thoracostomy is just a brief lived solution for a compromised affected person with a rigidity pneumothorax. A chest tube is usually indicated for a pneumothorax created by needle decompression. Approximately three fourths of sufferers with a traumatic hemothorax can be managed by tube thoracostomy and volume alternative alone. Patients must be provided with careful directions for follow-up inside 12 hours to 2 days, relying on the circumstances. Patients could also be admitted for remark in the occasion that they reside distant from emergency companies or follow-up care is taken into account unreliable (good consensus). Some of the panel members argued in opposition to observation alone due to a report of deaths with this method. The lung ought to be reexpanded through the use of a small-bore catheter (14 Fr) or placement of a 16- to 22-Fr chest tube (good consensus). Catheters or tubes may be attached both to a Heimlich valve (good consensus) or to a water seal gadget (good consensus) and could also be left in place till the lung expands towards the chest wall and the air leaks have resolved. If the lung fails to reexpand quickly, suction must be utilized to a water seal gadget. Some sufferers with empyema can be treated with serial thoracenteses, but most would require steady drainage with a chest tube. Usually, diagnostic thoracentesis is performed first to assess the fluid for signs of an infection. Thick pus on thoracentesis, positive Gram stain, fluid glucose degree lower Massive hemothorax, >1000-mL to 1500-mL preliminary drainage Continued bleeding >300 to 500 mL within the first hour >200 mL/hr for the first three or extra hours Increasing size of the hemothorax on a chest movie Persistent hemothorax after two functioning tubes are placed Clotted hemothorax Large air leak stopping efficient ventilation Persistent air leak after placement of a second tube or inability to fully increase the lung that is meant to be a information and clinical judgment should always be used. Insert an extended closed Kelly clamp excessive of the rib, and stab into the pleural house. Once the Kelly clamp is within the pleural area, open it extensively to create a lease within the parietal pleura. Generally, the tube is left in place until the pleural drainage fluid turns into clear yellow and accumulates lower than a hundred and fifty mL in 24 hours. In steady sufferers, relative contraindications embody anatomic problems such as the presence of a quantity of pleural adhesions, emphysematous blebs, or scarring. Coagulopathic patients should be evaluated for alternative of clotting elements before any invasive process. The goal is to open the pleural house rapidly to allow any accrued air to escape and decompress the chest cavity. This may be completed with a scalpel and forceps, as is done at the beginning levels of a thoracostomy. Place the catheter within the second intercostal area on the midclavicular line on the facet with diminished breath sounds or on either side if the prognosis is unclear. If unable to get hold of entry to this landmark, or if unsuccessful in penetrating into the pleural house, an alternate website in the fourth or fifth intercostal area on the midaxillary line can be used. Remove the needle, but go away the angiocatheter in place to create a simple pneumothorax. Needle decompression causes an open pneumothorax and typically needs to be converted to an open thoracostomy. A large-bore needle/catheter combination is used to puncture the parietal pleura and establish the presence of fluid or air in the pleural area. The needle could be positioned anywhere in the pleural space, however traditionally at the identical sites used for tube thoracostomy: the anterior second intercostal area in the midclavicular line or the anterior axillary line in the fourth or fifth interspace. The needle is positioned in order that it enters over the rib to avoid neurovascular injury. The needle is then withdrawn whereas leaving the catheter behind to create a easy open pneumothorax. The procedure can be carried out both with or without the syringe hooked up to the catheter. This is simply a temporary therapeutic maneuver for a pressure pneumothorax, and a chest tube must also be inserted. Sterile drapes 10- to 20-mL syringe and various needles (for local anesthesia) Local anesthetic (1% to 2% lidocaine) Antiseptic solution Scalpel with a No. When a affected person has an open chest wound in the prehospital setting, a three-sided occlusive dressing to cover the wound can create an appropriate one-way valve whereas providing wound safety. Similar to different one-way valve mechanisms, this dressing allows air to escape throughout expiration, but prevents air from coming into the chest cavity during inspiration. Use a sterile dressing, such as petrolatum-impregnated gauze, that extends 6 to 8 cm beyond the wound in all directions. Additionally, there are a number of commercially out there vented and nonvented chest seals that may be applied over the wound. In the case of the nonvented chest seal, the supplier could must release or "burp" the chest seal if the patient begins to reveal signs and/or signs again according to pressure physiology after they were efficiently needle decompressed. Instruct the patient to deeply inhale, carry out a Valsalva maneuver, or cough when you place the dressing. Chest tubes are manufactured so that the radiopaque lines are interrupted at the stage of the most proximal drainage hole. Emergency Department Treatment Equipment the usual instruments for a tube thoracostomy tray are listed in Box 10. The most simple needs are a scalpel, a big (Kelly) clamp, and the thoracostomy (chest) tube. Thoracostomy tubes are clear plastic tubes of assorted diameters which may be open at both ends. Tube sizes vary from 12 to forty two Fr, with smaller tubes used for smaller pneumothoraces and larger (a minimum of 36 Fr) tubes for hemothorax and empyema. The second intercostal area, midclavicular line, is the popular site for needle aspiration or catheter insertion (A). The fourth or fifth intercostal area, midaxillary to anterior axillary line (lateral to the pectoralis muscle and breast tissue), is most popular for a chest tube (B). In an overweight woman an assistant has to retract the breast upward to determine landmarks and keep away from low placement.
Purchase reglan 10 mg free shipping
If a stylet is used gastritis diet vegetarian buy discount reglan 10 mg on line, place it in the tube and bend it into the form of an open J with the distal finish terminating in a mild hook gastritis tums reglan 10 mg generic without a prescription. If the clinician has sufficiently lengthy fingers, place them posterior to the arytenoids to act as a "backstop" for the tube, to both keep away from esophageal passage and assist in laryngeal placement. A variation of the technique of digital intubation has been described for intubating a newborn. In addition, emergency physicians incessantly use paralytics to facilitate orotracheal intubation. A prehospital collection of 66 digitally intubated sufferers demonstrated an 89% success fee. Introduced by Butler and Cirillo in 1960,337 the technique has undergone a quantity of current modifications which have enhanced its value as a means of creating a definitive airway when more conventional methods have failed. The tracheal tube is cradled between the index and middle fingers and guided into the glottic opening. Indications embody trismus, ankylosis of the jaw or cervical spine, upper airway lots or swelling, unstable cervical backbone injuries, and maxillofacial trauma. It can be utilized to convert transtracheal needle ventilation (see Chapter 6) into a definitive airway. If fast control of the airway is needed, contemplate different alternate strategies together with a cricothyrotomy because retrograde intubation takes a number of minutes to set up and carry out. The tube is guided by using only the index finger to palpate the epiglottis and laryngeal inlet. Bend the top of the tube and moisten both the tube and the finger with sterile water. Use the index finger of the nondominant hand to comply with the tongue posteriorly and palpate the epiglottis and paired arytenoids. The tube will encounter delicate resistance because it enters the trachea, and palpation of the tube via the trachea provides further affirmation of right placement. A styletted tube, formed in the type of a J, is often desired until familiarity with the procedure is achieved. Equipment Materials include (1) local anesthetic and skin preparation materials, (2) an 18-gauge needle, (3) a 60-cm epidural catheterneedle mixture or an 80-cm (0. Complications the risk associated with esophageal intubation is all the time present, and the potential for esophageal misplacement is increased in comatose or cardiac-arrest sufferers. If used in patients with a gag reflex, induction of emesis with aspiration is a danger. A high incidence of left primary stem intubation was famous in a cadaveric study,336 but medical confirmation is lacking. Procedure and Technique Locate the three essential anatomic landmarks by palpation: hyoid bone, thyroid cartilage, and cricoid cartilage. Aspirate air to affirm place of the tip of the needle throughout the lumen of the larynx. An various entry point is the high trachea, usually through the subcricoid house, with the identical steps getting used as described for the cricothyroid membrane. If the wire is discovered within the hypopharynx, grasp it with the Magill forceps and draw it out via the mouth. Remove the needle from the neck and secure the tip of the wire on the puncture website with a hemostat. The subsequent steps will depend upon whether or not a plastic sheath, also referred to as an obturator, is on the market. Threading the wire by way of the aspect port allows the tip of the tube to protrude 1 cm past the purpose at which the wire enters the larynx. Because retrograde intubation is a blind approach, it may be troublesome to decide whether the tube has entered the trachea or is impeded by more proximal buildings. If unsure, pull the tube again 2 cm, rotate it ninety levels counterclockwise, and then readvance the tube. If a sheath is on the market, after greedy the wire from the mouth, thread the plastic sheath over the wire till it involves relaxation towards the anterior laryngeal wall. If any resistance at the arytenoids or vocal cords is encountered, pull the tube back 1 to 2 cm and rotate it 90 degrees counterclockwise. One advantage of the antegrade sheath is that it lies freely within the larynx, allowing more posterior passage by way of the widest distance between the cords. A 90� counterclockwise tube rotation and jaw traction will help the tube cross into the laryngeal inlet. The potential for hemorrhage is minimized by taking care to puncture the cricothyroid membrane in its decrease half to keep away from the cricothyroid artery. A small incidence of soft tissue an infection is reported with translaryngeal needle procedures, and ensuring that the wire is withdrawn from the mouth rather than the neck can minimize this downside. The last complication, failure to achieve intubation, has been mitigated by addition of the antegrade sheath over the wire. A method of changing the tube without losing control of the tracheal lumen is most well-liked. This may be achieved by passing a information down the defective tube, withdrawing the tube whereas leaving the information in place, and introducing a new tube over the guide and into the trachea. Tracheal Retrograde Intubation 1 Place a saline-filled needle via the cricothyroid membrane. B) Pass the antegrade sheath over the wire into the trachea whereas maintaining both ends of the wire taut. This is the important portion of the process as a result of solely a small portion of the sheath is in the trachea. Bougies are typically simpler to locate in the airway cart and intubators are extra familiar with their use. They most often happen when patients abruptly pull out their very own tube or during transport. Procedure and Technique Before the procedure, sedate and restrain the affected person correctly. While making use of cricoid strain, withdraw the defective tube over the guide, and take care to not dislodge the information when eradicating the tube. At this juncture, it may be helpful to carry out a jaw-thrust or chin-lift maneuver to facilitate passage via the pharynx. If this occurs, withdraw the tube 1 to 2 cm, rotate it 90 levels counterclockwise, and then readvance it. After the tube is visualized clearly within the trachea, take away the information, inflate the cuff, and ventilate the patient. Although the definition of a tough airway will change as our capability to visualize the laryngeal inlet continues to enhance, the problem of emergency airways will persist. Mastery of technique, advance preparation of equipment, and experience in medical decision-making are important. Scenario visualization and superior simulation fashions can provide a superb means of practicing the tough choice making and technical maneuvers essential for efficient emergency airway management. Russell T, Ng L, Nathan E, et al: Supplementation of ordinary preoxygenation with nasal prong oxygen or machine oxygen flush during a simulated leak situation.
Purchase reglan 10 mg free shipping
Doing so will anesthetize the lungs without correctly anesthetizing the vocal cords gastritis diet chocolate buy reglan 10 mg free shipping. Nebulize a 4-mL volume of a 4% lidocaine resolution over a period of approximately 5 minutes gastritis diet soy milk reglan 10 mg order with amex. Bourke and colleagues152 reported reaching consistently good topical anesthesia with this technique, though their sufferers were typically premedicated with combinations of opioids and sedatives. There has been an growing de-emphasis on the importance of premedications previous to intubation. Hebert and Daniel Thomas incidence of surgical airways has decreased even additional since the creation of adjunctive intubation techniques. Both surgical cricothyrotomy and needle cricothyrotomy entail puncture of the cricothyroid membrane by way of the overlying skin to achieve entry to the airway. Tracheostomy differs from cricothyrotomy in that the incision is made between two of the tracheal rings. The time period jet air flow usually refers to low-frequency jet ventilation with oxygen from a wall source versus high-frequency jet ventilation from a devoted jet ventilator. Although not often required, the 1�5 cartilage offers the attachment for the vocal ligaments. Superior to the thyroid cartilage and connecting it to the hyoid bone is the thyroid membrane, which permits passage of the superior laryngeal vessels and the interior department of the superior laryngeal nerve through its laterally located foramina. The cricoid cartilage varieties the inferior border of the cricothyroid membrane and is the one fully circumferential cartilaginous construction of the larynx. It is composed of a broad posterior segment that tapers laterally to kind a slim anterior arch. Identify the cricothyroid membrane between the previously talked about constructions as a shallow melancholy measuring roughly 9 mm longitudinally and 30 mm transversely. If the depression is obscured by delicate tissue swelling, estimate the situation of the cricothyroid membrane at approximately 2 to three cm inferior to the laryngeal prominence or 4 fingerbreadths above the sternal notch. The cricothyroid arteries branch from the superior thyroid arteries and may kind a small anastomotic arch traversing the superior aspect of the cricothyroid membrane. The external branch of the superior laryngeal nerve runs along the lateral aspect of the larynx and innervates the cricothyroid muscles inferior to the membrane. The isthmus of the thyroid gland most frequently overlies the second and third tracheal rings, although an aberrant pyramidal lobe of the gland could extend just superior to the cricothyroid membrane. The anterior attachments of the vocal cord structures are protected by the thyroid cartilage11,12. When time and the scientific state of affairs permit, it could be applicable to attempt to intubate a number of times with conventional laryngoscopy or to attempt different intubation strategies. Emergency choices are subject to controversy and differ on a case-by-case evaluation, but alternatives to cricothyrotomy embrace bag-valve-mask air flow, the gum elastic bougie, and laryngeal mask airways. At some level, further attempts at intubation become futile and the benefits of a surgical airway outweigh the risks related to ongoing hypoxia. The membrane is bordered superiorly by the thyroid cartilage and inferiorly by the cricoid cartilage. The lateral features of the cricothyroid membrane are partially lined by the cricothyroid muscle tissue, but the central triangular portion is subcutaneous, which makes it an ideal location to entry the airway. Identify the cricothyroid membrane by locating the outstanding thyroid cartilage superior to it. The thyroid cartilage consists of two lateral laminae that be part of at an acute angle within the midline to kind the laryngeal prominence. Cricothyrotomy Indications Inability to preserve >90% saturation between intubation attempts or after three attempts Inability to bag-mask-valve ventilate the affected person between intubation attempts or after three attempts Multiple attempts at endotracheal intubation fail to safe the airway after failed rescue maneuvers. Higher scores are related to poor glottic visualization and tough intubation. It classifies the degree that the faucial pillars, taste bud, and uvula could be visualized. Additional indicators of a difficult airway include obesity, oropharyngeal edema, hemorrhage, and laryngospasm22�25 (Box 6. In anticipation of a failed airway, it could be reasonable to mark the cricothyroid membrane using ultrasound steering to prepare for the potential of a cricothyrotomy. The actual age at which surgical cricothyrotomy could be carried out is controversial and never properly outlined. Various textbooks list the lower age restrict from 5 years30 to 10 years31 or 12 years. Some authors also identify tracheal transection or low tracheal obstruction (below the cricoid) as absolute contraindications to cricothyrotomy due to the necessity to safe the airway below the injury33 (Box 6. Equipment the gear essential to perform a conventional surgical cricothyrotomy includes a scalpel with a No. In addition, the sterile tray may embrace a syringe and lidocaine with epinephrine for local anesthesia, sterile drapes or towels, antiseptic preparation solution, 4 � 4-cm sterile gauze, scissors, hemostats, and suture material. Surgical cricothyrotomy can safely and efficiently be carried out with minimal cervical backbone motion. Prepare the pores and skin of the anterior aspect of the neck with antiseptic resolution and create a sterile area with the use of drapes or towels. If the patient is awake or responding to ache, give a subcutaneous and translaryngeal injection of lidocaine with epinephrine as a local anesthetic. Wear sterile gloves and take standard precautions by wearing a mask, goggles, and robe. In a follow-up report in 1989, Erlandson and colleagues38 emphasized the importance of constructing an preliminary vertical pores and skin incision and utilizing a relatively small (No. These modifications have usually been accepted and are commonly described as part of the traditional approach. Stabilize the larynx with the nondominant hand by greedy each side of the lateral thyroid cartilage with the thumb and center finger. In shorter or more obese sufferers, or in patients with neck swelling, these landmarks may be more difficult to establish by palpation alone. Immobilize the larynx together with your nondominant hand and palpate the cricothyroid membrane with your index finger. With the index finger of the nondominant hand, palpate the cricothyroid membrane by way of the incision. Place the nondominant index finger into the stoma momentarily and trade the scalpel for the tracheal hook. Rotate the deal with cephalad whereas greedy the inferior border of the thyroid cartilage with it. Ask an assistant to present upward traction or present traction yourself by passing the handle of the hook to the nondominant hand. With the dominant hand, place the ideas of the Trousseau dilator into the opening in the membrane with the spreading motion oriented initially in the longitudinal or vertical airplane so that the deal with is dealing with horizontal or perpendicular to the direction of the neck. This instrument works opposite that of most odd devices, corresponding to hemostats. Hold the handles of the Trousseau dilator with the nondominant hand and rotate the handle ninety degrees until the deal with is vertical or parallel to the neck. If the dilator is left horizontal, the blades of the dilator might impede passage of the tracheostomy tube into the trachea.
10 mg reglan free shipping
It is essential to acknowledge that extra sinister pathology can current as a seizure; consequently gastritis pain treatment reglan 10 mg generic with mastercard, a careful historical past and examination are paramount for protected decision-making gastritis translation buy 10 mg reglan mastercard. Epidemiology and threat components Between 1 and 5 years of age, ~1 in 20 youngsters will undergo a febrile convulsion. Lennox�Gastaut, Dravet, infantile spasms) Pathophysiology An activation or inhibition of neurones can result in an imbalance being created, so causing an total web excitation paroxysmal discharge. The brain area affected dictates the signs related to the seizure (see Table 12. Consciousness may be affected in focal seizures, however is at all times affected during generalized seizures. Risk components: � Learning disability � First-degree relative affected There are many aetiologies which can trigger epilepsy, which include: � Idiopathic � Genetic syndromes similar to tuberous sclerosis, Rett syndrome and Prader�Willi syndrome � Metabolic disease � Mitochondrial illness � Intracranial infection � Post-traumatic � Electrolyte disturbance (high glucose, low Ca2+, low Mg2+, high or low Na+) Rapid diagnosis � common (1 & 2) and rare (3�5) epilepsy syndromes 1. Onset in adolescence and characterized by myoclonic, tonic-clonic and absence seizures. Infantile spasms (West syndrome): 3�9 months of age and characterized by transient myoclonic spasms after waking. Characterized by automatisms, tonic/clonic/atonic/ myoclonic, affecting particular area of physique. These typically final for 1�3 minutes and are characterised by an initial inflexible phase (in which the child falls to the floor), by which the child may bite their tongue. This is followed by a rhythmic, jerking part, during which the child may lose control of the bladder and bowels. It selfterminates and the kid resumes what they were doing, with no post-ictal part. Investigation and diagnosis Hx � Ask fastidiously about occasions before, throughout and after the episode: � Warnings Carbamazepine or lamotrigine Sodium valproate or lamotrigine Ethosuximide or sodium valproate Sodium valproate (or levetiracetam if unsuitable) Sodium valproate (or lamotrigine if unsuitable) 201 12. Onset is 6�18 months of age, with spontaneous resolution occurring between 4 and eight years old. Hx � A typical sequence of occasions following minor injury/upset, resulting in unconsciousness. Epidemiology and risk factors Tic disorders might happen in <20% of kids and family historical past will increase threat by 10�100x. Rapid prognosis � Tourette syndrome Diagnostic standards (clinical): � 2 motor and 1 vocal tic � Present for 12 months � Onset <18 years old � Tics not caused by different situations. Term Ataxia Athetosis Chorea Dyskinesia Dystonia Myoclonus Torticollis Tremor Definition Unsteady, broad-based gait Writhing, slow actions Unpredictable, irregular, non-rhythmic movements A broad time period for any involuntary, abnormal movement Repetitive twisting motion and postures, often sustained Brief, sudden involuntary actions A dystonia specifically affecting the neck Rhythmic oscillation of a body half 12. It is often associated with sleepwalking and characterized by sudden arousal from sleep through the non-rapid eye motion section. Sleepwalking is seen in ~5% of kids and is most prevalent between three and 7 years of age. Conservative measures to guarantee safety are essential: Remove breakable objects Remove trip hazards Windows locked Sleep on backside bunk Fit safety gates 12. There is an increased incidence in these with mental well being and personality disorders. This often leads to pointless diagnostic procedures, which may be invasive, that the patient typically accepts with equanimity. Pathophysiology Headaches can be categorized as main (attributable to a headache disorder) or secondary (due to one other underlying disease). Pathophysiology Lateral ventricle (Monro) Third ventricle (aqueduct of Sylvius) Fourth ventricle (Luschka (�2) and Magendie (�1)) Subarachnoid space (arachnoid granulations) Dural venous sinuses. Definitive remedy is surgical decompression via placement of a ventricular shunt. Ventricular catheter Catheter tunnelled beneath the skin Incision Incision into peritoneal cavity Peritoneal cavity. These genes serve as tumour suppressors, and aberrations subsequently predispose to the development of tumours inside the nervous system � these are normally benign, but may be malignant. Rapid analysis � different neurocutaneous issues � Sturge�Weber syndrome: angiomas affecting the pores and skin and meninges. Diagnosis and investigation Often presents as seizures (due to cortical tubers), but clinical manifestations vary. Pathophysiology Damage to the immature brain occurring between ~24/40 gestation (prenatal; 75%), delivery (perinatal; 10%) and <3 y/o (postnatal; 15%). This results in the next: Prenatal (75%) Impaired development of the brain Damage to the immature mind Perinatal (10%) Death of brain tissue Postnatal (15%) If the lesion impacts: � the motor cortex or pyramidal tracts higher motor neurone signs (~80%) � basal ganglia or cerebellum decrease motor neurone signs (~20%). Characterized by: � Abnormal, involuntary, writhing actions (hyperkinesia), mainly affecting the face and extremities � Facial grimacing and drooling � Feeding and speech impairment � Hypotonia � Normal reflexes ii. Characterized by: � Prolonged, gradual, repetitive actions, which can have an result on the whole body region � Abnormal posturing � Hypotonia � Normal reflexes 3. Characterized by: � Loss of coordinated muscular contraction clumsiness, impaired balance and abnormal gait � Hypotonia � Intention tremor Regional involvement Spastic Global (total body) involvement Dyskinetic Ataxia Hemiplegia Normal Mild involvement Severe involvement Diplegia Pyramidal Quadriplegia Athetoid Dystonic Extrapyramidal Ataxic. Here we talk about how to perform a structured evaluation of these kids and address some frequent circumstances presenting on this way. Rarely, the cause is direct inoculation (from penetrating injury or surgery) or spread from adjoining osteomyelitis. Epidemiology and threat components Prematurity (immune function) Delivered by C-section Invasive procedures 50% of children affected are <2 years old (Table 13. Diabetes mellitus Sickle cell disease Immunocompromise Penetrating injury/open fracture Table thirteen. Within the major curve, the vertebral bodies additionally rotate, pushing the spinous processes towards the concave side. The aetiologies can be divided into the next: Structural � Idiopathic (~70% of all scoliosis cases) � Congenital � Neuromuscular � neuropathic. Investigation and prognosis Hx � Back pain is widespread � Concern about cosmesis Ex � Increased kyphosis � Further elevated by bending forwards � Full neurological evaluation required ( Management � <60�: observation and physiotherapy � 60�80�: bracing � Surgery indicated if: >80�, extreme pain or neurological deficit 235 13. We present a broad method to the work-up of these children and summarize the pertinent findings of crucial circumstances. Investigation and prognosis Hx A comprehensive historical past, as detailed in Chapter 1, with specific consideration paid to: � the duration and pattern of joint involvement ( Pathophysiology: production of autoantibodies in opposition to nuclear antigens and the formation of immune complexes, which result in tissue injury/organ injury. Hx: non-specifically unwell (fatigue, fevers, weight) with pain in multiple joints. Pathophysiology: an autoimmune situation causes vasculopathy with subsequent muscle and skin ischaemia. Interestingly, although autosomal dominant, 80% of circumstances are due to a de novo mutation in utero. Anaemia develops because of insufficient consumption (diet), insufficient absorption (chronic inflammation.
Reglan 10 mg discount fast delivery
In particular gastritis diet list order 10 mg reglan overnight delivery, direct measurement of arterial strain throughout pulseless electrical rhythms may assist discriminate between a extreme shock state and otherwise nonresuscitatable status follicular gastritis definition 10 mg reglan purchase visa. The current part discusses indirect blood strain monitoring; intraarterial techniques are considered elsewhere. Discussion of the particular use of the Doppler device for measurement of pulse and blood stress and for measurement of orthostatic blood strain and modifications in pulse observe this part. Despite an affiliation between the absence of hypotension and the presence of a radial pulse or between hypotension and the absence of each radial and femoral pulses within the setting of trauma, the variability in individual responses prohibits the use of this parameter as an absolute gauge of blood pressure. This follow, though typically the only feasible technique of obtaining any worth in a noisy surroundings, poses a significant potential for error. According to the American heart Association guidelines, the sphygmomanometer cuff ought to be an applicable dimension for the patient to guarantee an correct studying. This printed figure of the ideal width, when studied in a validation evaluate, may be greater, as much as roughly 50%. All three forms of manometers are convenient for bedside use, although the mercury gravity column should be placed vertically to ensure correct measurements. An aneroid manometer uses a metal bellows that elongates with the appliance of pressure. This elongation is mechanically amplified and transmits the movement to the indicator needle. Mercury columns could require the addition of mercury to convey the edge of the meniscus to the zero mark. The air vent or filter on the top of the mercury column should also be checked for clogging. An aneroid manometer must be calibrated towards a mercury column a minimum of yearly. Automatic sphygmomanometers may enhance physiologic monitoring with their alarm and self-cycling capabilities. They offer oblique arterial blood strain measurement with little ache and with out the dangers related to invasive arterial traces. Oscillometric blood strain screens detect movement of the blood stress cuff transmitted from the underlying artery. In adult sufferers, quite a few studies have focused on the reliability of auscultatory versus automated blood pressure measurements. Mercury column versus Dinamap readings showed elevated disparity when systolic blood strain was higher than one hundred forty mm hg, the range at which accuracy ought to be most rigorously sought to appropriately establish hypertension. In basic, automated blood pressure units yield greater systolic and decrease diastolic blood pressure. Automatic sphygmomanometer validation is a type of calibration and deserves quality control and traceability to ensure correct outcomes. The technique is straightforward and correct when the tools is properly maintained, calibrated, and utilized by clinicians who observe accepted standards. The affected person may be lying or sitting, so long as the location of measurement is on the degree of the proper atrium and the arm is supported. These adjustments are thought to be dependent on the mechanical properties of the arteries themselves and never related to hydrostatic pressure alone. Once properly inflated, palpate immediately over the artery and deflate the cuff at a price of 2 to three mm hg/sec. Report the preliminary appearance of arterial pulsations because the palpable blood pressure. This apply, known as the Riva-Rocci palpatory technique, has shown combined ends in yielding correct estimations of blood strain. One research determined that the average underestimation of systolic blood stress was 6 mm hg. Measurement of arterial strain by palpation and Doppler yields only estimates of systolic blood strain. The sometimes said contraindications to the acquisition of upper arm blood strain (limitation after mastectomy, and so forth. Complications Complications of indirect blood strain measurements are minimal when the right process is adopted. Inadvertent extended software of an inflated blood strain cuff may end in falsely elevated diastolic stress and ischemia distal to the location of software. Diastolic blood stress is defined as the point at which the sounds disappear (Korotkoff section V). It is greatest to auscultate over the brachial artery due to accepted standardization of the measured values. Alternative sites embrace the radial, popliteal, posterior tibial, or dorsalis pedis arteries, though any totally compressible extremity artery could also be used. Studies evaluating direct and indirect blood strain measurements have demonstrated good correlation between these methods. Forearm measurements may be obtained more simply, though correlation to normal proximal upper extremity values has been controversial. An earlier study confirmed fair correlation to a brachial cuff measurement (within 20 mm hg in 86% of systolic measurements and 94% of diastolic measurements). Individual components that influence blood strain embrace physique posture, emotional or painful stimuli, environmental influences, vasoactive meals or medications, and the state of muscular and cerebral exercise. Exercise and sustained isometric muscular contraction enhance blood stress in proportion to the energy of the contraction. A regular diurnal sample of blood strain consists of a rise throughout the day with a major, rapid decline during early, deep sleep. Children older than 2 years are considered hypotensive when systolic blood stress is less than eighty mm hg. Most adults are thought-about hypotensive if systolic blood pressure is decrease than 90 mm hg, however some individuals normally exhibit a systolic pressure in that range. In the aged, the presence of normotension within defined or published limits is in all probability not reassuring. Ausculta- tion till the manometer reading approaches zero ought to forestall misinterpretation. Extremes of blood strain, both hypotension and hypertension, have been found to be components contributing to measurement errors in critically unwell pediatric patients. Predictably, falsely excessive readings for noninvasive versus invasive measurements have been obtained in hypotensive patients and falsely low values in hypertensive states. Take a second or third studying, with 2 minutes of deflation between recordings, and procure an average when untimely contractions or atrial fibrillation are present. The solely approach to fight these errors is to first be cognizant of practices contributing to them. Nurses had been capable of correctly establish defective equipment 58% of the time, assess cuff measurement 57% of the time, determine acceptable inflation strain 29% of the time, notice the appropriate deflation price 62% of the time, and decide appropriate arm positioning 14% of the time. For example, if the blood strain is 120/80 mm hg, the pulse strain is 40 mm hg. A narrowed pulse pressure (20 mm hg) may be a manifestation of hypovolemia, increased peripheral vascular resistance (as seen in early septic shock), or decreased stroke volume. A narrowed pulse pressure is classically famous in aortic stenosis and pericardial tamponade.
Cheap 10 mg reglan otc
While most of these veins are valveless gastritis diet bland purchase reglan 10 mg online, latest proof suggests that some valves do exist in variable numbers in a few of these veins gastritis ultrasound discount 10 mg reglan with amex. An ascending lumbar vein from the higher stomach cavity collects venous blood segmentally and often from the left renal vein; it is a crucial connection between these stomach caval veins and the azygos system within the thorax. A variety of mediastinal veins exist in the posterior mediastinum and drain the diaphragm, pericardium, esophagus, and primary bronchi. Ascending lumbar vein (left) Posterior intercostal veins (left 8�12th) Esophageal veins Mediastinal veins Superior phrenic veins (left) 2. Inferior vena cava Ascending lumbar vein (right) Posterior intercostal veins (right 5�11th) Esophageal veins Mediastinal veins Pericardial veins Bronchial veins (right) Right superior intercostal vein three. About midway within the thorax, the hemiazygos vein crosses the midline and drains into the azygos vein (3), although the hemiazygos normally maintains its reference to the accent hemiazygos vein as nicely. Veins tend to join with one another the place attainable, and many connections are small, variable, and not readily recognizable. Flow in the azygos system of veins is stress dependent; as a end result of the veins are primarily valveless, the flow can go in both direction. As with different regional veins, the variety of veins of the azygos system may be variable. Thoracic Lymphatics he thoracic lymphatic duct begins in the stomach on the cisterna chyli (found between the abdominal aorta and the right crus of the diaphragm), ascends via the posterior mediastinum posterior to the esophagus, crosses to the left of the median airplane at roughly the T5-T6 vertebral level, and empties into the venous system at the junction of the left inner jugular and left subclavian veins. Lymph from the left hemithorax and left lung typically drains into tributaries that empty into the thoracic duct. Lymph 138 Inferior deep cervical (internal jugular) nodes Thoracic duct Paratracheal nodes Superior and inferior tracheobronchial nodes Posterior mediastinal nodes Intercostal nodes Posterior parietal nodes Chapter three Thorax mesoderm types the stroma of each lung. By 6 months of gestation, the alveoli are mature sufficient for gas trade, but the manufacturing of surfactant, which reduces surface pressure and helps forestall alveolar collapse, will not be suicient to support respiration. Early Embryonic Vasculature Toward the end of the third week of improvement, the embryo establishes a primitive vascular system to meet its rising needs for oxygen and nutrients. Blood leaving the embryonic heart enters a sequence of paired arteries known as the aortic arches, which are associated with the pharyngeal arches. Some of the blood enters the vitelline arteries to provide the long run bowel (still the yolk sac at this stage), and some passes to the placenta by way of a pair of umbilical arteries, the place gases, nutrients, and metabolic wastes are exchanged. Blood getting back from the placenta is oxygenated and carries vitamins again to the center through the one umbilical vein. Blood also returns to the guts by way of the next veins: Vitelline veins: drain blood from yolk sac; will turn out to be the portal system draining the gastrointestinal tract by way of the liver. Aortic Arches Blood pumped from the primitive embryonic coronary heart passes into aortic arches that are associated with the pharyngeal arches. Note that the third, fourth, and sixth pairs of embryonic aortic arches are the most important contributors to arteries that can persist within the fetus and neonate. Bulbus cordis: receives ventricular blood and passes it to the truncus arteriosus. Truncus arteriosus: receives blood from the bulbus cordis and passes it to the aortic arch system for distribution to the lungs and body. Shortly after birth, when the strain of the left atrium exceeds that of the right atrium (blood now passes into the lungs and returns to the left atrium, raising the strain on the left side), the 2 septae are pushed together and fuse, thus forming the fossa ovalis of the postnatal heart. Fetal Circulation he sample of fetal circulation is one of gas exchange and nutrient/metabolic waste exchange across the placenta with the maternal blood (but not the change of blood cells), and distribution of oxygen and nutrient-rich blood to the tissues of the fetus. Various shunts enable fetal blood to largely bypass the liver (not needed for metabolic processing in utero) and lungs (not needed for gas trade in utero) so that the blood may acquire direct access to the left aspect of the heart and be pumped into the fetal arterial system. At or shortly after delivery, these shunts close, ensuing within the normal sample of pulmonary and systemic circulation observed postnatally. Approximately 80% of instances are perimembranous (occur where the muscular septum and membranous septum of the endocardial cushion should fuse). This results in a left-to-right shunt, which can precipitate congestive coronary heart failure. Chapter three Thorax one hundred forty five three Clinical Focus 3-23 Atrial Septal Defect Atrial septal defects make up approximately 10% to 15% of congenital cardiac anomalies. Most of those defects are ostium secundum defects from incomplete closure of the foramen ovale. For smaller atrial septal defects, a percutaneous transcatheter approach utilizing a septal occluder may be deployed and secured. The Amplatzer Septal Occluder is deployed from its delivery sheath, forming two discs, one for either aspect of the septum, and a central waist out there in varying diameters to seat on the rims of the atrial septal defect. Atrial septum Inferior vena cava Right atrium After sizing the defect, the supply sheath is used to insert the gadget into the left atrium and deploy it on the defect. Tricuspid valve Right ventricle Once the left atrial disc and part of the connecting waist are deployed, the device is rigorously pulled back until the left atrial disc touches the septum and the waist is within the septal defect. Left ventricle the best atrial disc is deployed and the location of the occluder is checked by echocardiography. This ends in a postnatal shunt of blood from the aorta into the pulmonary trunk, which may lead to congestive heart failure. A steady murmur normally is obvious over the left sternal border to slightly below the clavicle (see Clinical Focus 3-17). Pulmonary trunk Pathophysiology of patent ductus arteriosus Decreased systemic circulate Left-to-right shunt via patent ductus arteriosus Increased pulmonary move (pulmonary volume overload) Left ventricular hypertrophy Chapter three Thorax 147 3 Clinical Focus 3-25 Repair of Tetralogy of Fallot Tetralogy of Fallot often results from a maldevelopment of the spiral septum that normally divides the truncus arteriosus into the pulmonary trunk and aorta. The stenotic pulmonary outflow tract is widened by inserting a patch into the wall (pericardial), thus increasing the amount of the subpulmonic stenosis and/or the pulmonary artery stenosis. Two drainage tubes inserted since one could clog, however immediate or early thoracotomy could additionally be essential to arrest bleeding. Chronic cough may cause conjunctival bleeding, epistaxis, vomiting, stress urinary incontinence, rib fractures, disc herniation, hernias, esophageal rupture, and cardiac arrhythmias. Infections in the type of pneumonia account for one sixth of all deaths in the United States. Staphylococcal pneumonia Severe staphylococcal pneumonia complicating endocarditis, with abscess formation, empyema, vegetations on tricuspid valve, and emboli in branches of pulmonary artery Pneumococcal pneumonia Lobar pneumonia; right higher lobe Right higher lobe and segment of right lower lobe pneumonia 148. These vague or confusing signs could contribute to a delayed or missed prognosis. Percutaneous coronary intervention offers entry to the vein graft, often by way of the femoral artery. By this method, one might introduce distal safety and thrombectomy gadgets, corresponding to balloons for expansion or stents, which scale back the incidence of occlusion, embolization, and infarction in these patients with ischemia. Percutaneous coronary intervention: vascular entry Distal safety device Aorta Guide catheter Saphenous v. Guide catheter Stent delivery catheter with its balloon inflated and the stent expanded Stent in place Stenotic lesion Native vessel Occlusion balloon inflated Aspiration catheter aspirating atherosclerotic particles 148. Common portals of bacterial entry in bacterial endocarditis Dental infections Genitourinary infections Cutaneous infections Pulmonary infections Bloodstream Bicuspid aortic valve (congenital or acquired) Mild residual changes of rheumatic mitral valve disease Early vegetations of bacterial endocarditis at contact line of mitral valve Early vegetations of bacterial endocarditis on bicuspid aortic valve Common predisposing lesions Chapter 3 Thorax 148. Normal mitral valve Thickened, redundant valve leaflets and chordae tendineae Anterior anulus Posterior leaflet Chordae tendineae Papillary m. Left atrium Left ventricle Late systolic murmur following midsystolic click on (mitral prolapse) S1 A2 P2 Normal systole mitral valves coapt on ventricular side of mitral valve. Plane of mitral valve anulus Click Left ventricle Left atrium In mitral valve prolapse, mitral valve leaflets coapt on atrial aspect of the plane of the mitral anulus.
Reglan 10 mg line
Interventions If the patient is steady gastritis definition cause reglan 10 mg order line, an try to gastritis diet ����� reglan 10 mg buy lowest price visualize the bleeding site with direct visualization using a fiberoptic scope must be performed. Look for evidence of bleeding on the anterior tracheal wall at or under the sternal notch. If important tracheal bleeding or a clot is current, first hyperinflate the tracheostomy tube cuff with the 50-mL syringe to compress the artery towards the posterior sternal wall. Depending on the make and model of the tube, inflating the cuff with the entire 50 mL may not be potential. If the patient continues to bleed despite this maneuver, apply digital strain by way of the tracheal stoma to compress the anterior tracheal wall in opposition to the sternum. Digital strain is taken into account essentially the most dependable approach to stop hemorrhage and may provide management of bleeding during transport to the working room. The clinician must be cautious to not harm surrounding vasculature when making the incision. Minor Bleeding All bleeding from a tracheostomy site must be evaluated for a potentially life-threatening occasion. Consider endoscopic examination for complete analysis except a superficial bleeding website is confirmed. Minor bleeding is most likely the outcomes of irritated granulation tissue and is often confined to the pores and skin surrounding the stoma. Bloody secretions from the tracheostomy tube may symbolize tracheitis, bleeding operating down from the skin or thyroid, or superficial tracheal ulceration from tracheal suctioning or tracheal tube stress. Examine the stoma site and tube first in an try to find the source and quantify the quantity of blood loss. If the supply of bleeding is inside the stoma or from within the trachea, take away the tracheostomy tube if it was positioned greater than 7 days before the current event. Visualize the tracheal lumen, proximal finish of the trachea, and inner stoma with a nasopharyngoscope or a small pediatric laryngoscope. Do not try and take away clots within the trachea as a result of this will enhance the speed of hemorrhage. Prosthesis dislodgement, occlusion, or erosion secondary to an infection should be thought of in all sufferers with acute changes in voice manufacturing or decreased capacity to speak. In secure sufferers, administration of prosthesis issues must be referred to a specialist, most commonly an otolaryngologist. Interventions For exterior or stomal bleeding, start with local irrigation to discover the supply of the bleeding. Most incisional or stomal bleeding can be stopped by making use of direct pressure for three to 5 minutes. Application of absorbable hemostatic materials may enhance the finish result of direct pressure application. Following tube substitute, suction rigorously to affirm decision of the bleeding and to determine secondary sources of bleeding. Placement of a nasogastric tube will help in the identification of gastrointestinal bleeding. If the affected person has undergone radiation therapy, study the area above the level of the tracheostomy stoma, where mucosal injury secondary to radiation damage could also be the cause of blood within the tracheal secretions. Many patients with continual obstructive pulmonary disease, pulmonary fibrosis, sleep apnea, lung most cancers, and 1-antitrypsin deficiency are candidates for outpatient use of supplemental oxygen. Although nasal cannula oxygenation is easy to administer, it has a number of unwanted facet effects, including drying of the nasal mucosa, epistaxis, ear discomfort, contact dermatitis from the oxygen tubing, and dry throat. These techniques scale back issues, improve patient comfort, and enhance compliance. The catheter is held in place by a subcutaneous tract, and is inserted into the decrease a part of the trachea. Low-flow oxygen (2 to 10 L/min) is supplied directly to the trachea by a slim (7- to 11-Fr) catheter. Typically, an 11-cm catheter sits in the trachea with its tip 1 to 2 cm above the carina. The catheter is held in place by a skinny band or necklace via two openings within the flange. The surgical process is often done in an outpatient setting with the affected person under local anesthesia. Developed within the 1980s, it may be performed as a main or secondary process after laryngectomy or different pharyngeal surgeries. The mucosa in segments of the pharyngeal esophagus vibrates in response to airflow, thereby creating speech. Once the tracheocutaneous fistula has epithelialized, the catheter may be inserted. After the tract has fully matured, most sufferers can change their catheter at house. One milliliter of sterile saline is instilled into the catheter, and a cleaning rod is inserted as far as possible. The cleansing rod is inserted and extracted 3 times to take away secretions and encrustations from the lumen of the catheter. The stoma must be cleaned twice every day and inspected totally for signs of infection. All patients ought to be given supplemental oxygen by nasal cannula throughout catheter maintenance procedures. Adequate humidification, cleaning, and systemic hydration will assist scale back the incidence of mucous blockage. Early complications (developing inside 3 weeks after the procedure) occur in roughly 30% of sufferers and embrace bleeding, infection, pneumothorax, costochondritis, and dislodgement (which could be attributable to coughing). Life-threatening airway obstruction ensuing from the formation of a large mucous ball has been reported. Obstruction inside the catheter tubing could trigger a whistling sound from the oxygen tank humidifier. Always examine the patient for signs of subcutaneous air and catheter dislodgement. If routine broad-spectrum antibiotics are used by the patient, Candida infections can develop at the stoma. Such infections are more frequent in sufferers receiving systemic antibiotics or long-term corticosteroids or these with diabetes. Many patients with chondritis have a deep, indurated, nonfluctuant lump around the tract that might be tender to palpation. If important bleeding is recognized or suspected, seek the guidance of a specialist on an emergency basis and handle the airway definitively as clinically indicated (see the part on Major Bleeding). Manage pores and skin and pulmonary infections with the methods mentioned for tracheostomy care. Stents Tracheal stenosis and tracheomalacia are known problems of artificial airways. Management options embrace surgical procedure and placement of silicone stents in the trachea. Morbidly obese sufferers are significantly in danger for lifethreatening complications associated to tracheostomy.
Discount reglan 10 mg line
If attempts continue to lead to esophageal misplacement gastritis symptoms pain 10 mg reglan order with mastercard, the following maneuver could lead to profitable tracheal intubation gastritis vs gerd 10 mg reglan cheap amex. This method could additionally be significantly helpful in sufferers with cervical spine injury as a result of it requires no manipulation of the top or neck. The suction catheter will typically move simply into the trachea; the cuff could be deflated and the tube advanced into the trachea. A common mistake is exerting an extreme amount of pressure on the ring, which can lead to the tube curling up before the larynx and preventing advancement. There has been a case report of an Endotrol tube "kinking" on the point of sharpest curvature and inflicting difficulty with suctioning however no problems with ventilation. This is frequently profitable as a end result of the vocal cords are broadly kidnapped during inhalation. Assess laryngeal anesthesia, and if topical and nebulized lidocaine has already been administered with out success, contemplate transcricothyroid anesthesia. B, Rotation of tube 90 levels counterclockwise orients the bevel of the tip posteriorly and permits passage into the larynx. The tracheal tube is then handed over the suction catheter, and the catheter is removed. This maneuver orients the bevel of the tube posteriorly and incessantly ends in successful passage. It will usually move via the larynx with out difficulty, and the tube can then be advanced over the catheter. Withdraw the tube 2 cm, rotate it slightly away from the bulge, after which readvance it. Severe epistaxis was encountered in solely 5 of 300 cases reported by Danzl and Thomas. B, Once breath sounds are heard, the cuff is inflated with 15 mL of air and readvanced into the laryngeal inlet. Once seated within the inlet, the cuff is deflated and the tube advanced into the trachea. Digital intubation could be significantly helpful in situations with poor lighting, irregular patient positioning. Advantages embrace velocity and ease of placement, immunity to constraints visualizing the larynx, and little neck movement. The tip of the epiglottis should be palpated eight to 10 cm from the nook of the mouth in common adults. Use of a stylet within the tube is elective, but the largest reported collection had good success and not using a stylet. Ooi R, Pattison J, Joshi P, et al: Pre-oxygenation: the Hudson masks as an alternative approach. Hayes-Bradley C, Lewis A, Burns B, et al: Efficacy of Nasal Cannula Oxygen as a Preoxygenation Adjunct in Emergency Airway Management. Miguel-Montanes R, Hajage D, Messika J, et al: Use of high-flow nasal cannula oxygen remedy to prevent desaturation during tracheal intubation of intensive care sufferers with mild-to-moderate hypoxemia. Lane S, Saunders D, Schofield A, et al: A prospective, randomised controlled trial comparing the efficacy of pre-oxygenation in the 20� head-up vs supine position. Wimalasena y, Burns B, Reid C, et al: Apneic oxygenation was related to decreased desaturation charges throughout speedy sequence intubation by an Australian helicopter emergency medicine service. Shiga T, Wajima Z, Inoue T, et al: Predicting tough intubation in apparently regular patients: a meta-analysis of bedside screening take a look at efficiency. Salimi A, Farzanegan B, Rastegarpour A, et al: Comparison of the higher lip chew check with measurement of thyromental distance for prediction of adverse intubations. Honarmand A, Safavi M, Ansari N: A comparison of between hyomental distance ratios, ratio of top to thyromental, modified Mallamapati classification check and upper lip bite test in predicting troublesome laryngoscopy of patients undergoing common anesthesia. In Calder I, Pearce A, editors: Core subjects in airway administration, Cambridge, 2005, Cambridge University Press, p 113. Herbstreit F, Fassbender P, Haberl H, et al: Learning endotracheal intubation using a novel videolaryngoscope improves intubation skills of medical college students. Konrad C, Schupfer G, Wietlisbach M, et al: Learning manual skills in anesthesiology: is there a really helpful variety of instances for anesthetic procedures Neelakanta G: Cricoid pressure is effective in stopping esophageal regurgitation. Ellis Dy, Harris T, Zideman D: Cricoid strain in emergency division speedy sequence tracheal intubations: a risk-benefit analysis. Combes X, Leroux B, Jabre P, et al: Out-of-hospital rescue oxygenation and tracheal intubation with the intubating laryngeal masks airway in a morbidly obese affected person. Pediatric Emergency Medicine Committee of the American College of Emergency Physicians. Noguchi T, Koga K, Shiga y, et al: the gum elastic bougie eases tracheal intubation while applying cricoid pressure in comparability with a stylet. Aoyama K, Takenaka I, Sata T, et al: Cricoid stress impedes positioning and air flow through the laryngeal masks airway. Asai T, Barclay K, Power I, et al: Cricoid stress impedes placement of the laryngeal masks airway and subsequent tracheal intubation through the mask. Asai T, Barclay K, Power I, et al: Cricoid pressure impedes placement of the laryngeal masks airway. Brimacombe J: Laryngeal masks anesthesia: priciples and follow, Philadelphia, 2005, Saunders. Brimacombe J, White A, Berry A: Effect of cricoid strain on ease of insertion of the laryngeal masks airway. Harris T, Ellis Dy, Foster L, et al: Cricoid pressure and laryngeal manipulation in 402 pre-hospital emergency anaesthetics: essential security measure or a hindrance to fast safe intubation In Brunnings W, editor: Direct laryngoscopy, bronchoscopy, and esophagoscopy, London, 1912, Balliere, Tindall, & Cox, p 110. Morton T, Brady S, Clancy M: Difficult airway tools in English emergency departments. Chou H-C, Chong K-M, Sim S-S, et al: Real-time tracheal ultrasonography for affirmation of endotracheal tube placement during cardiopulmonary resuscitation. Shippey B, Ray D, McKeown D: Case series: the McGrath videolaryngoscope-an initial medical analysis. Nouruzi-Sedeh P, Schumann M, Groeben H: Laryngoscopy via Macintosh blade versus GlideScope: success fee and time for endotracheal intubation in untrained medical personnel. Shippey B, Ray D, McKeown D: Use of the McGrath videolaryngoscope in the management of adverse and failed tracheal intubation. Uya A, Spear D, Patel K, et al: Can Novice Sonographers Accurately Locate an Endotracheal Tube With a Saline-filled Cuff in a Cadaver Model Muslu B, Sert H, Kaya A, et al: Use of sonography for fast identification of esophageal and tracheal intubations in grownup sufferers. Sim S-S, Lien W-C, Chou H-C, et al: Ultrasonographic lung sliding sign up confirming correct endotracheal intubation throughout emergency intubation. Lyon M, Walton P, Bhalla V, et al: Ultrasound detection of the sliding lung signal by prehospital important care providers. Bissinger U, Lenz G, Kuhn W: Unrecognized endobronchial intubation of emergency patients. Niforopoulou P, Pantazopoulos I, Demestiha T, et al: Video-laryngoscopes within the adult airway management: a topical evaluate of the literature. Jungbauer A, Schumann M, Brunkhorst V, et al: Expected difficult tracheal intubation: a potential comparability of direct laryngoscopy and video laryngoscopy in 200 patients.