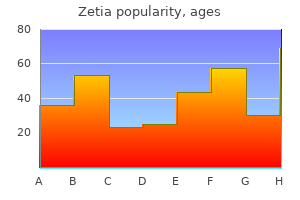
Zetia dosages: 10 mg
Zetia packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
10 mg zetia discount
A rolled gauze bandage impregnated with calamine ideal cholesterol ratio for an individual zetia 10 mg buy otc, zinc oxide cholesterol test device cheap zetia 10 mg with mastercard, glycerin, sorbitol, gelatin, and magnesium aluminum silicate is first utilized with graded compression from the forefoot to slightly below the knee. The subsequent layer consists of a 4-in-wide continuous gauze dressing adopted by an outer layer of elastic wrap, also utilized with graded compression. The bandage becomes stiff after drying, and the rigidity may aid in stopping edema formation. The purported advantages of multilayered dressings embrace maintenance of compression for a longer period of time, more even distribution of compression, and higher absorption of wound exudates. However, the efficacy of multilayered dressings depends on the wrapping strategy of healthcare personnel. Several forms of skin substitutes are commercially out there or beneath clinical study in the United States. Their mechanism of action in therapeutic venous ulcers is unsure; however, they might function delivery autos for numerous development factors and cytokines essential in wound healing. Apligraf is a commercially out there bilayered dwelling pores and skin assemble that carefully approximates human skin to be used within the treatment of venous ulcers. It incorporates a protecting stratum corneum and a keratinocyte-containing epidermis overlying a dermis consisting of dermal fibroblasts in a collagen matrix. Apligraf skin graft material supplied as a disk on an agarose gel nutrient medium. The disk is easily dealt with and applied and conforms to irregularly contoured ulcer beds. A potential randomized examine comparing multilayer compression remedy alone to treatment with Apligraf in addition to multilayered compression remedy has been performed to assess the efficacy of Apligraf in the therapy of venous ulcers. The median time to complete ulcer closure was significantly shorter in patients handled with Apligraf (61 days vs. The ulcers that confirmed the greatest benefit with the living skin construct have been ones that had been large and deep (>1000 mm2) or have been longstanding (>6 months). No evidence of rejection or sensitization has been reported in response to Apligraf software. Surgical/Interventional Treatment of Chronic Venous Insufficiency Perforator Vein Ligation. Incompetence of the perforating veins connecting the superficial and deep venous techniques of the lower extremities has been implicated within the development of venous ulcers. The traditional open approach described by Linton in 1938 for perforator vein ligation has a high incidence of wound complications and has largely been deserted. The patient is positioned on the working table with the affected leg elevated at 45� to 60�. The knee is then flexed, and two small incisions are made within the proximal medial leg away from areas of maximal induration at the ankle. Laparoscopic trocars are then positioned, and the subfascial dissection is carried out with a mix of blunt and sharp dissection. After completion of the process, the leg is wrapped in a compression bandage for five days postoperatively. Adjunctive procedures, primarily superficial vein stripping, have been performed in 72% of sufferers. Ulcer recurrence was predicted to be 16% at 1 yr and 28% at 2 years by life desk evaluation. These outcomes are just like those achieved in some studies with compression remedy alone. Superficial venous surgery had no additive impact to compression alone in the healing of a venous ulcer but considerably lowered venous ulcer recurrence at 4 years. However, in patients with a mixture of superficial and deep vein valvular incompetence, the addition of deep vein valvular reconstruction theoretically may 934 improve ulcer therapeutic. These strategies consist of restore of existing valves, transplant of venous segments from the arm, transposition of an incompetent vein onto an adjoining competent vein, and implantation of cryopreserved vein segments including competent valves. Successful long-term outcomes of 60% to 80% have been reported for venous valve reconstructions by internal suture repair. The outcomes for venous transposition are similar to those for valve transplantation. Axillary node dissection leading to lymphedema of the arm is the commonest explanation for secondary lymphedema within the United States. Other causes of secondary lymphedema embody radiation therapy, trauma, an infection, and malignancy. Globally, filariasis (an an infection caused by Wuchereria bancrofti, Brugia malayi, and Brugia timori) and environmental exposure to minerals in volcanic soil resulting in podoconiosis in barefoot populations are the most typical causes of secondary lymphedema. It appears attainable to place percutaneous stents within the iliac veins with close to 100 percent technical success and glorious patency of the stent out to four years. The limb size will increase all through the day and reduces to some extent over the course of the night when the patient is recumbent. In the lower extremity, the swelling classically includes the dorsum of the foot, and the toes have a squared-off appearance. Repeated infection ends in additional lymphatic damage, worsening existing disease. The scientific presentation of cellulitis ranges from subtle erythema and worsening of edema to a rapidly progressive delicate tissue infection with systemic toxicity. If the signs are delicate, distinguishing lymphedema from other causes of leg swelling can be tough. However, sufferers with advanced venous insufficiency sometimes have lipodermatosclerosis within the gaiter area, pores and skin ulceration, and/or varicose veins. It is caused by anatomic and or physiologic abnormalities corresponding to lymphatic hypoplasia, functional insufficiency, or absence of lymphatic valves. The unique classification system, described by Allen, relies on the purpose for the lymphedema. Primary lymphedema is additional subdivided into congenital lymphedema, 6 lymphedema praecox, and lymphedema tarda. Congenital lymphedema may involve a single lower extremity, multiple limbs, the genitalia, or the face. The edema sometimes develops earlier than 2 years of age and could additionally be related to particular hereditary syndromes (Turner syndrome, Milroy syndrome, KlippelTr�naunay-Weber syndrome). Lymphedema praecox is the most common type of primary lymphedema, accounting for 94% of cases. Lymphedema praecox is much extra frequent in girls, with the gender ratio favoring girls 10:1. The onset is during childhood or the teenage years, and the swelling involves the foot and calf. The diagnostic modalities mentioned within the following sections have restricted use in medical follow. They are invasive and tedious and rarely change the administration of a affected person with lymphedema. Lymphoscintigraphy has turn out to be probably the most generally used diagnostic test to identify lymphatic abnormalities.
Effective 10 mg zetia
It has a sensitivity and specificity of 95% and 89% cholesterol in egg white discount 10 mg zetia with amex, respectively hdl good cholesterol foods 10 mg zetia buy amex, at detecting choledocholithiasis. It is the check of choice in evaluating the affected person with suspected malignancy of the gallbladder, the extrahepatic biliary system, or close by organs, particularly, the head of the pancreas. Computed tomography scan of the higher stomach from a affected person with most cancers of the distal common bile duct. Once the endoscopic cholangiogram has shown ductal stones, sphincterotomy and stone extraction could be carried out, and the common bile duct cleared of stones. In the arms of specialists, the success price of common bile duct cannulation and cholangiography is >90%. Schematic diagram of percutaneous transhepatic cholangiogram and drainage for obstructing proximal cholangiocarcinoma. A plastic catheter has been handed over the wire, and the wire is subsequently removed. Long wire positioned via the catheter and advanced past the tumor and into the duodenum. Typical complications corresponding to bile duct perforation, minor bleeding from sphincterotomy or lithotripsy, and cholangitis have been described. Endoscopic Ultrasound Endoscopic ultrasound requires a special endoscope with an ultrasound transducer at its tip. The results are operator dependent, however offer noninvasive imaging of the bile ducts and adjacent structures. For unknown causes, some patients progress to a symptomatic stage, with biliary colic attributable to a stone obstructing the cystic duct. Symptomatic gallstone disease might progress to complications related to the gallstones. Several research have examined the chance of creating biliary colic or growing significant problems of gallstone disease. Complicated gallstone illness develops in 3% to 5% of symptomatic patients per year. Over a 20-year interval, about two thirds of asymptomatic patients with gallstones remain symptom free. For elderly patients with diabetes, for individuals who will be isolated from medical look after prolonged periods of time, and in populations with increased danger of gallbladder most cancers, a prophylactic cholecystectomy may be advisable. This view exhibits the course of the extrahepatic bile ducts (arrow) and the pancreatic duct (arrowheads). A schematic picture displaying the side-viewing endoscope in the duodenum and a catheter in the widespread bile duct. The main natural solutes in bile are bilirubin, bile salts, phospholipids, and ldl cholesterol. Gallstones are classified by their cholesterol content as either cholesterol stones or pigment stones. In Western international locations, about 80% of gallstones are cholesterol stones and about 15% to 20% are black pigment stones. Most different cholesterol stones comprise variable quantities of bile pigments and calcium, but are always >70% cholesterol by weight. Whether pure or of blended nature, the frequent main event within the formation of ldl cholesterol stones is supersaturation of bile with cholesterol. Therefore, high bile cholesterol levels and cholesterol gallstones are thought-about as one disease. Cholesterol solubility is dependent upon the relative focus of ldl cholesterol, bile salts, and lecithin (the primary phospholipid in bile). Supersaturation virtually always is caused by ldl cholesterol hypersecretion rather than by a decreased secretion of phospholipid or bile salts. Cholesterol is held in answer by micelles, a conjugated bile salt-phospholipid-cholesterol complex, in addition to by the cholesterol-phospholipid vesicles. The presence of vesicles and micelles in the same aqueous compartment allows the movement of lipids between the 2. Vesicular phospholipids are incorporated into micelles more readily than vesicular ldl cholesterol. Therefore, vesicles might turn out to be enriched ste rol ole 60 s% 2 or extra phases forty % n ithi Lec Ch 40 60 Mo le 20 Cholesterol Stones. A given point represents the relative molar ratios of bile salts, lecithin, and ldl cholesterol. The space labeled "micellar liquid" shows the vary of concentrations discovered in keeping with a transparent micellar solution (single phase), the place cholesterol is absolutely solubilized. The shaded space immediately above this region corresponds to a metastable zone, supersaturated with cholesterol. Bile with a composition that falls above the shaded space has exceeded the solubilization capacity of ldl cholesterol and precipitation of cholesterol crystals happens. In the supersaturated bile, cholesterol-dense zones develop on the surface of the cholesterol-enriched vesicles, leading to the looks of ldl cholesterol crystals. Pigment stones comprise <20% ldl cholesterol and are darkish due to the presence of calcium bilirubinate. Otherwise, black and brown pigment stones have little in frequent and ought to be thought of as separate entities. They are shaped by supersaturation of calcium bilirubinate, carbonate, and phosphate, most frequently secondary to hemolytic issues such as hereditary spherocytosis and sickle cell disease, and in those with cirrhosis. Excessive ranges of conjugated bilirubin, as in hemolytic states, result in an increased rate of manufacturing of unconjugated bilirubin. When altered situations lead to elevated ranges of deconjugated bilirubin in bile, precipitation with calcium happens. In Asian international locations such as Japan, black stones account for a a lot higher share of gallstones than in the Western hemisphere. Brown stones are often <1 cm in diameter, brownishyellow, delicate, and infrequently mushy. They may type both in the gallbladder or within the bile ducts, often secondary to bacterial infection attributable to bile stasis. Precipitated calcium bilirubinate and bacterial cell bodies compose the major a part of the stone. Bacteria such as Escherichia coli secrete -glucuronidase that enzymatically cleaves bilirubin glucuronide to produce the insoluble unconjugated bilirubin. It precipitates with calcium, and together with dead bacterial cell our bodies, types soft brown stones within the biliary tree. Brown stones are typically discovered within the biliary tree of Asian populations and are associated with stasis secondary to parasite infection. In Western populations, brown stones happen as main bile duct stones in patients with biliary strictures or different frequent bile duct stones that cause stasis and bacterial contamination. About two thirds of patients with gallstone disease current with continual cholecystitis characterized by recurrent attacks of pain, often inaccurately labeled biliary colic. The ache develops when a stone obstructs the cystic duct, resulting in a progressive increase of rigidity in the gallbladder wall. The mucosa is initially regular or hypertrophied, but later turns into atrophied, with the epithelium protruding into the muscle coat, leading to the formation of the so-called Aschoff-Rokitansky sinuses.
Safe zetia 10 mg
Although mechani4 cal valves are extremely durable cholesterol test tube color generic zetia 10 mg otc, they require everlasting anticoagulation remedy to mitigate the otherwise high threat of valve thrombosis and thromboembolic sequelae cholesterol definition biology online zetia 10 mg generic mastercard. Conversely, patients with other indications for systemic anticoagulation, similar to other risk components for thromboembolism. Additionally, patients with renal failure, on hemodialysis, or with hypercalcemia experience accelerated degeneration of bioprosthetic valves, and are thus, really helpful to receive mechanical prostheses. The potential to avoid the hazards of serious bleeding complications spurred the development of valve prostheses using organic supplies, which obviate the necessity for systemic anticoagulation therapy. As tissue valves are naturally less thrombogenic, the attendant yearly dangers of each thromboembolic and anticoagulation-related complications are considerably less than with mechanical valves. However, organic valves are more prone to degeneration, especially when implanted in the mitral place, in youthful sufferers, and in sufferers in renal failure, on hemodialysis, or with hypercalcemia. Bileaflet mechanical valves have demonstrated glorious move traits, low risks of late valverelated issues, including valve failure, and are presently probably the most commonly implanted kind of mechanical valve prosthesis on the earth. When managed appropriately, the yearly thromboembolic and bleeding risks in these sufferers are 1% to 2%, and 0. A xenograft valve is one implanted from one other species, corresponding to porcine xenograft valves, or manufactured from tissue corresponding to bovine pericardium. Stented valves are the most generally implanted, and the preferred valve in the United States is a stented bovine pericardial valve. The chief drawback of stented tissue valves is a smaller efficient orifice area, which increases the transvalvular gradient. Homograft valves from human cadavers, also called allografts, have been used for aortic valve alternative for the rationale that method was originally described over 50 years ago. Following harvest, these valves are sterilized using an antibiotic solution, and subsequently saved in fixative or cryopreserved. Additionally, the construction of homograft valves is naturally low-profile, permitting for larger effective valve orifices and decrease postoperative transvalvular gradients compared with stented xenograft valves. In addition to potential concerns with sturdiness, performance of the Ross procedure has also been restricted by its technical complexity, and the increased surgical danger associated with double valve substitute. The thickened, fused leaflets of the diseased mitral valve are viewed by way of a left atriotomy. Despite its advantages for the patient, valve repair is generally extra technically demanding than valve replacement, and should sometimes fail. Both the suitability of the patient for valve repair and the talent and experience of the surgeon performing the operation are important when contemplating valve restore within the individual patient. The diploma of mitral stenosis ought to be decided preoperatively, as these pathological features might help determine the timing and kind of intervention to perform. The elevated left atrial stress is subsequently transmitted to the pulmonary venous system, causing pulmonary edema as the hydrostatic stress within the vessels exceeds the plasma oncotic stress. Decreased pulmonary venous compliance exacerbates the pulmonary venous hypertension, though a concomitant decrease in microvascular permeability may preclude pulmonary edema within the continual setting. The secondary obstruction to flow brought on by reactive pulmonary arterial hypertension could serve to protect towards pulmonary edema, but in addition exacerbates the intractable decrease in cardiac output that develops as stenosis worsens. Although rheumatic coronary heart illness is related to a transmural pancarditis, pathological fibrosis of the valves results primarily from the endocarditic process. Left ventricular construction and function are typically preserved, however, owing to the protecting impact of the stenotic valve. The sudden opening of the thickened, nonpliable valve with left atrial contraction produces a gap snap, followed by a diastolic rumble caused by rapid entry of blood into the left ventricle. The murmur, classically known as the auscultatory triad, is greatest heard on the apex. Associated mitral and tricuspid insufficiencies are heard as a pansystolic murmur radiating to the axilla, and a systolic murmur at the xiphoid course of, respectively. Chest X-ray findings may include enlargement of the left atrium and pulmonary artery, making a double contour behind the best atrial shadow, and obliterating the traditional concavity between the aorta and left ventricle. The characteristic auscultatory findings additionally embody an apical systolic murmur which is variably transmitted to the axilla or the left sternal border, relying on the situation of the pathology. Findings according to pulmonary hypertension incessantly indicate late-stage illness. The papillary muscular tissues are reattached to the annulus and, if potential, the posterior leaflet along with its associated subvalvular structures are preserved. The annulus is subsequently sized, and an acceptable mitral prosthesis is implanted utilizing pledgeted horizontal mattress sutures. The annular sutures could also be positioned from the atrial to the ventricular side, seating the valve intra-annularly, or from the ventricular to the atrial aspect, seating the valve in a supra-annular place. When inserting the mattress sutures, care must be taken to keep inside the annular tissue, as excessively deep bites could trigger damage to critical structures such because the circumflex coronary artery posterolaterally, the atrioventricular node anteromedially, or the aortic valve anterolaterally. Traditionally, a median sternotomy incision is used; nonetheless, the left atrium may also be approached by way of minimally-invasive incisions, similar to a minithoracotomy or a partial sternotomy. The commissure is then carefully incised in a barely anterior path 2 to 3mm at a time, making sure with each extension of the incision that the chordae tendineae stay hooked up to the commissural leaflets. The commissurotomy is generally stopped 1 to 2mm from the annulus where the leaflet tissue thins, indicating the transition to regular commissural tissue. The papillary muscles are subsequently examined and incised as needed in order to maximize the mobility of the leaflets. After the commissurotomy is complete, and the associated chordae tendineae and papillary muscle tissue are mobilized, leaflet mobility is assessed. The anterior leaflet is grasped with forceps and introduced through its full range of motion. If subvalvular restriction or leaflet rigidity is identified, additional division or excision of fused chordae and debridement of calcium may be essential. Valve replacement could additionally be more appropriate if extensive secondary mobilization is required. At the tip of the process, competence of the valve is assessed with injection of cold saline into the ventricle. Open surgical commissurotomy has an operative threat of <1%, and has been proven to have good long term results, with freedom from reoperation as high as 88. On opening the atrium, the endocardium is examined for a jet lesion, a roughened space caused by a regurgitant jet hanging the wall, in order to higher localize the area of valvular insufficiency. The subvalvular equipment and particular person leaflets are subsequently examined, and areas of prolapse, restriction, fibrosis, and calcification are identified. Leaflet perforations are generally repaired primarily, or with a pericardial patch. Excision of the diseased leaflet tissue extends down in direction of but generally not to the mitral annulus. After repair has been accomplished, valvular competency is evaluated by injecting saline into the ventricle with a bulb syringe and assessing leaflet mobility and apposition. If focal insufficiency is recognized in other areas, extra procedures are performed. The anterior leaflet could additionally be repaired via chordal shortening, chordal transposition, artificial chordal replacement, and triangular resection of the anterior leaflet. During chordal transposition, a resected portion of the posterior leaflet with connected chordae is transposed onto the prolapsed portion of the anterior leaflet to provide structural support, and adopted with posterior leaflet repair as described above.
Zetia 10 mg cheap without a prescription
This storage is made attainable due to the exceptional absorptive capacity of the gallbladder is there cholesterol in quail eggs zetia 10 mg order without a prescription, as the gallbladder mucosa has the best absorptive power per unit area of any construction in the physique cholesterol hoax 10 mg zetia cheap mastercard. It quickly absorbs sodium, chloride, and water towards important concentration gradients, concentrating the bile as a lot as 10-fold and resulting in a marked change in bile composition. This fast absorption is considered one of the mechanisms that stop an increase in strain within the biliary system beneath normal circumstances. Gradual rest in addition to emptying of the gallbladder in the course of the fasting interval also plays a job in maintaining a comparatively low intraluminal stress in the biliary tree. The epithelial cells of the gallbladder secrete at least two important merchandise into the gallbladder lumen: glycoproteins and hydrogen ions. The mucosal glands within the infundibulum and the neck of the gallbladder secrete mucus glycoproteins which are believed to shield the mucosa from the lytic action of bile and to facilitate the passage of bile through the cystic duct. This mucus makes up the colorless "white bile" seen in hydrops of the gallbladder resulting from cystic duct obstruction. The transport of hydrogen ions by the gallbladder epithelium leads to a decrease within the gallbladder bile pH. The acidification promotes calcium solubility, thereby stopping its precipitation as calcium salts. Gallbladder filling is facilitated by tonic contraction of the sphincter of Oddi, which creates a pressure gradient between the bile ducts and the gallbladder. In response to a meal, the gallbladder empties by a coordinated motor response of gallbladder contraction and sphincter of Oddi leisure. Other hormonal and neural pathways also are involved in the coordinated motion of the gallbladder and the sphincter of Oddi. Defects within the motor activity of the gallbladder are thought to play a task in cholesterol nucleation and gallstone formation. The vagus nerve stimulates contraction of the gallbladder, and splanchnic sympathetic stimulation is inhibitory to its motor activity. Parasympathomimetic medication contract the gallbladder, whereas atropine results in rest. Neurally mediated reflexes link the sphincter of Oddi with the gallbladder, abdomen, and duodenum to coordinate the circulate of bile into the duodenum. Antral distention of the stomach causes each gallbladder contraction and relaxation of the sphincter of Oddi. Hormonal receptors are positioned on the smooth muscle tissue, vessels, nerves, and epithelium of the gallbladder. Vasoactive intestinal polypeptide inhibits contraction and causes gallbladder rest. Patients handled with somatostatin analogues and those with somatostatinoma have a excessive incidence of gallstones, presumably because of the inhibition of gallbladder contraction and emptying. Other hormones similar to substance P and enkephalin affect gallbladder motility, but the physiologic role is unclear. The sphincter of Oddi is about 4 to 6 mm in length and has a basal resting strain of about 13 mmHg above the duodenal stress. On manometry, the sphincter exhibits phasic contractions with a frequency of about four per minute and an amplitude of 12 to 140 mmHg. In 1924, the diagnosis of gallstones was improved significantly by the introduction of oral cholecystography by Graham and Cole. During fasting, with the sphincter of Oddi contracted and the gallbladder filling. In response to a meal, the sphincter of Oddi relaxed and the gallbladder emptying. If related to an elevation of bilirubin, alkaline phosphatase, and aminotransferase, cholangitis should be suspected. Cholestasis, an obstruction to bile flow, is characterised by an elevation of bilirubin. In patients with biliary colic or chronic cholecystitis, blood exams will usually be regular. Ultrasound will present stones in the gallbladder with sensitivity and specificity of >90%. Stones are acoustically dense and mirror the ultrasound waves again to the ultrasonic transducer. The affected person has acute cholecystitis if a layer of edema is seen throughout the wall of the gallbladder or between the gallbladder and the liver in affiliation with localized tenderness. When a stone obstructs the neck of the gallbladder, the gallbladder might turn out to be very massive, however thin walled. The extrahepatic bile ducts are additionally well visualized by ultrasound, aside from the retroduodenal portion. Dilation of the ducts in a affected person with jaundice establishes an extrahepatic obstruction as a cause for the jaundice. Frequently, the location and, typically, the trigger of obstruction could be determined by ultrasound. Small stones in the common bile duct frequently get lodged at the distal end of it, behind the duodenum, and are, due to this fact, troublesome to detect. A dilated frequent bile duct on ultrasound, small stones in the gallbladder, and the clinical presentation enable one to assume that a stone or stones are inflicting the obstruction. Periampullary tumors may be tough to diagnose on ultrasound, but beyond the retroduodenal portion, the extent of obstruction and the trigger may be visualized fairly nicely. Ultrasound can be useful in evaluating tumor invasion and flow in the portal vein, an necessary guideline for resectability of periampullary and pancreatic head tumors. Obese patients, sufferers with Oral Cholecystography Once thought of the diagnostic process of selection for gallstones, oral cholecystography has largely been changed by ultrasonography. Stones are noted on a film as filling defects in a visualized, opacified gallbladder. Oral cholecystography is of no worth in sufferers with intestinal malabsorption, vomiting, obstructive jaundice, and hepatic failure. Biliary scintigraphy provides a noninvasive evaluation of the liver, gallbladder, bile ducts, and duodenum with both anatomic and practical info. Uptake by the liver is detected inside 10 minutes, and the gallbladder, the bile ducts, and the duodenum are visualized inside 60 minutes in fasting subjects. The major use of biliary scintigraphy is in the analysis of acute cholecystitis, which appears as a nonvisualized gallbladder, with immediate filling of the widespread bile duct and duodenum. Evidence of cystic duct obstruction on biliary scintigraphy is very diagnostic for acute cholecystitis. False-positive results are elevated in sufferers with gallbladder stasis, as in critically sick patients and in sufferers receiving parenteral diet. Filling of the gallbladder and customary bile duct with delayed or absent filling of the duodenum indicates an obstruction on the ampulla. Biliary leaks as a complication of surgery of the gallbladder or the biliary tree can be confirmed and frequently localized by biliary scintigraphy. Through the catheter, a cholangiogram could be performed and therapeutic interventions carried out, similar to biliary drain insertions and stent placements.
10 mg zetia purchase amex
These superficial ulcers are as much as cholesterol levels lower naturally buy zetia 10 mg without prescription 3 mm in diameter and are surrounded by a halo 1154 of erythema cholesterol test kit uk cheap 10 mg zetia free shipping. These granulomas are noncaseating and can be present in each areas of energetic disease and apparently normal gut, in any layer of the bowel wall, and in mesenteric lymph nodes. Linear or serpiginous ulcers could type when multiple ulcers fuse in a course parallel to the longitudinal axis of the gut. With transverse coalescence of ulcers, a cobblestoned look of the mucosa may arise. Serosal involvement results in adhesion of the infected bowel to other loops of bowel or other adjoining organs. Transmural irritation can also result in fibrosis with stricture formation, intra-abdominal abscesses, fistulas, and, rarely, free perforation. The presence of fat wrapping correlates well with the presence of underlying acute and continual inflammation. It can be necessary to keep in thoughts that though ulcerative colitis is a illness of the colon, it could be associated with inflammatory adjustments in the distal ileum (backwash ileitis). There is substantial overlap amongst these disease patterns in individual sufferers, however. The onset of signs is insidious, and once current, their severity follows a waxing and waning course. The scientific severity of a few of these manifestations, corresponding to erythema nodosum and peripheral arthritis, are correlated with the severity of intestinal irritation. The severity of different manifestations, such as pyoderma gangrenosum and ankylosing spondylitis, bear no apparent relationship to the severity of intestinal inflammation. The diagnosis is normally established with endoscopic findings in a patient with a compatible medical historical past. The analysis ought to be considered in those presenting with acute or continual stomach pain, particularly when localized to the right lower quadrant, continual diarrhea, proof of intestinal inflammation on radiography or endoscopy, the invention of a bowel stricture or fistula arising from the bowel, and proof of irritation or granulomas on intestinal histology. These infectious enteritides are most incessantly identified in immunocompromised patients but can even occur in sufferers with regular immune perform. Typhoid enteritis brought on by Salmonella typhosa can result in overt intestinal bleeding and perforation, most often affecting the terminal ileum. The distal ileum and cecum are the most common websites of intestinal involvement by an infection because of Mycobacterium tuberculosis. Instead, the diagnosis is based on an entire assessment of the clinical presentation with confirmatory findings derived from radiographic, endoscopic, and generally pathologic exams. Colonoscopy with intubation of terminal ileum is the primary diagnostic device and might reveal focal ulcerations adjacent to areas of normal-appearing mucosa along with polypoid mucosal modifications that give a "cobblestone appearance. Contrast examinations of the small bowel and colon could reveal strictures or networks of ulcers and fissures. This picture was captured by a wi-fi capsule endoscope as it was touring by way of the small intestine. However, in acute shows, the analysis is typically made intraoperatively or during surgical evaluation. They are also used to treat patients with perianal disease, enterocutaneous fistulas, and energetic colonic disease. Aminosalicylates are associated with minimal toxicity and can be found in a big selection of formulations that permit for their delivery to specific regions of the alimentary tract. Patients with extreme active disease usually require intravenous administration of glucocorticoids. Some sufferers are unable to bear glucocorticoid tapering with out struggling recurrence of signs. The thiopurine antimetabolites azathioprine and its active metabolite, 6-mercaptopurine, have demonstrated efficacy in inducing remission, in sustaining remission, and in allowing for glucocorticoid tapering in glucocorticoid-dependent patients. These brokers are relatively secure however can induce bone marrow suppression and promote infectious issues. It is generally used for patients immune to commonplace therapy, to have the ability to assist taper steroid dosage. Whereas infliximab is a mouse-human chimeric antibody, the newer medicine in this group include adalimumab (Humira), which is a totally human antibody. Antibodies towards other targets on this inflammatory pathway have additionally been developed and are in varied phases of medical evaluation. In a randomized research of 24 sufferers, these receiving infliximab beginning 4 weeks after ileal resection had improved endoscopic and histologic scores at 1-year follow-up compared to those receiving placebo. Two to four weeks of remedy is required before improvements are seen, and sometimes long-term remedy is required to stop relapse. Failure of medical administration may be the indication for surgical procedure if symptoms persist regardless of aggressive therapy for several months or if signs recur every time aggressive remedy is tapered. Surgery must be thought of if medication-induced complications come up, particularly corticosteroid-related problems, corresponding to cushingoid features, cataracts, glaucoma, systemic hypertension, compression fractures, or aseptic necrosis of the femoral head. One of the most typical indications for surgical intervention is intestinal obstruction. Abscesses and fistulas are regularly encountered during operations carried out for intestinal obstruction in these patients, but are not often the one indication for surgical procedure. The presence of energetic disease is recommended by thickening of the bowel wall, narrowing of the lumen, serosal irritation and protection by creeping fat, and thickening of the mesentery. Segmental intestinal resection of grossly evident disease adopted by major anastomosis is the standard procedure of alternative. In a randomized prospective trial, the results of attaining 2-cm resection margins past grossly evident disease have been compared with reaching 12-cm resection margins. This technique allows for preservation of intestinal floor space and is particularly properly suited to sufferers with intensive illness and fibrotic strictures who could have undergone earlier resection and are at risk for growing short bowel syndrome. Any intraluminal ulcerations should be biopsied to rule out the presence of neoplasia. Depending on the length of the stricture, the reconstruction may be common in a way much like the HeineckeMickulicz pyloroplasty (for strictures <12 cm in length) or the Finney pyloroplasty (for longer strictures as much as 25 cm in length). For longer strictures, variations on the standard stricturoplasty, particularly the side-to-side isoperistaltic enteroenterostomy, have been advocated and used for strictures with imply lengths of 50 cm. Stricturoplasty is associated with recurrence charges which would possibly be no completely different from these associated with segmental resection. However, as knowledge on this complication are limited to anecdotes, this danger stays a theoretical one. Stricturoplasty is contraindicated in patients with intra-abdominal abscesses or intestinal fistulas. The presence of a solitary stricture comparatively close to a segment for which resection is deliberate is a relative contraindication. In basic, stricturoplasty is performed in circumstances where single or a number of strictures are recognized in diffusely concerned segments of bowel or where earlier resections have been carried out and maintenance of intestinal length is of great significance.
Turnera diffusa var. aphrodisiaca (Damiana). Zetia.
- Headaches, bedwetting, depression, nervous stomach, constipation, sexual problems, boosting mental and physical stamina, and other conditions.
- Are there safety concerns?
- What is Damiana?
- How does Damiana work?
- Are there any interactions with medications?
- Dosing considerations for Damiana.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96689
10 mg zetia purchase with visa
Risk components embrace vascular illness cholesterol in eggs paleo 10 mg zetia order, diabetes mellitus cholesterol test ldl size 10 mg zetia buy visa, vasculitis, hypotension, and tobacco use. In addition, ligation of the inferior mesenteric artery during aortic surgery predisposes to colonic ischemia. Although the splenic flexure is the most common web site of ischemic colitis, any phase of the colon may be affected. In mild instances, patients could have diarrhea (usually bloody) with out belly pain. With extra severe ischemia, intense stomach pain (often out of proportion to the medical examination), tenderness, fever, and leukocytosis are current. Peritonitis and/or systemic toxicity are signs of fullthickness necrosis and perforation. The analysis of ischemic colitis is usually based mostly on the medical history and physical examination. Plain films may reveal thumb printing, which ends from mucosal edema and submucosal hemorrhage. While sigmoidoscopy could reveal attribute darkish, hemorrhagic mucosa, the risk of precipitating perforation is excessive. For this cause, sigmoidoscopy is relatively contraindicated in any patient with vital stomach tenderness. Contrast research (Gastrografin or barium enema) are similarly contraindicated during the acute phase of ischemic colitis. Unlike ischemia of the small bowel, the overwhelming majority of sufferers with ischemic colitis may be treated medically. Bowel relaxation and broad-spectrum antibiotics are the mainstay of remedy, and 80% of sufferers will recuperate with this regimen. Hemodynamic parameters ought to be optimized, especially if hypotension and low flow appear to be the inciting trigger. Long-term sequelae embody stricture (10%�15%) and persistent segmental ischemia (15%�20%). Colonoscopy must be carried out after recovery to evaluate strictures and to rule out other diagnoses corresponding to inflammatory bowel illness or malignancy. Failure to improve after 2 to 3 days of medical management, progression of signs, and deterioration in clinical situation are indications for surgical exploration. Management ought to include instant cessation of the offending antimicrobial agent. Patients with gentle illness (diarrhea but no fever or stomach pain) could additionally be treated as outpatients with a 10-day course of oral metronidazole. Oral vancomycin is a second-line agent used in patients allergic to metronidazole or in sufferers with recurrent illness. More extreme diarrhea associated with dehydration and/or fever and stomach ache is greatest handled with bowel rest, intravenous hydration, and oral metronidazole or vancomycin. Recurrent colitis occurs in as much as 20% of patients and could also be handled by a longer course of oral metronidazole or vancomycin (up to 1 month) or rifaximin (a rapamycin derivative). Reintroduction of regular flora by ingestion of probiotics or stool transplantation has been instructed as a possible therapy for recurrent or refractory illness. Fulminant colitis, characterised by septicemia and/or evidence of perforation, requires emergent laparotomy. A variety of other infections with micro organism, parasites, fungi, or viruses might cause colonic inflammation. Less generally, Mycobacterium tuberculosis, Mycobacterium bovis, Actinomycosis israelii, or Treponema pallidum (syphilis) might cause colitis or proctitis. Parasitic infections corresponding to amebiasis, cryptosporidiosis, and giardiasis are also comparatively common. Fungal infections (Candida species, histoplasmosis) are extraordinarily rare in otherwise wholesome people. Most symptoms are nonspecific and include diarrhea (with or with out bleeding), crampy belly pain, and malaise. A thorough history could provide clues to the etiology (other medical circumstances, particularly immunosuppression; current travel or exposures; and ingestions). Diagnosis is normally made by identification of a pathogen in the stool, either by microscopy or tradition. Colitis is believed to end result from overgrowth of this organism after depletion of the conventional commensal flora of the intestine with using antibiotics. Immunosuppression, medical comorbidities, prolonged hospitalization or nursing home residence, and bowel surgery improve the risk. Diagnosis of this disease was traditionally made by culturing the organism from the stool. Detection of 1 or both toxins (either by cytotoxic assays or by immunoassays) has confirmed to be more rapid, delicate, and particular. The diagnosis can also be made endoscopically by detection of attribute ulcers, plaques, and pseudomembranes. Three hemorrhoidal 9 cushions are found in the left lateral, proper anterior, and right posterior positions. Hemorrhoids are thought to operate as a part of the continence mechanism and aid in complete closure of the anal canal at rest. Because hemorrhoids are a normal a half of anorectal anatomy, treatment is only indicated if they become symptomatic. Excessive straining, elevated belly pressure, and onerous stools enhance venous engorgement of the hemorrhoidal plexus and cause prolapse of hemorrhoidal tissue. External hemorrhoids are located distal to the dentate line and are coated with anoderm. Because the anoderm is richly innervated, thrombosis of an exterior hemorrhoid may cause important ache. A skin tag is redundant fibrotic skin at the anal verge, typically persisting because the residua of a thrombosed exterior hemorrhoid. Treatment of exterior hemorrhoids and skin tags is only indicated for symptomatic aid. Internal hemorrhoids are situated proximal to the dentate line and coated by insensate anorectal mucosa. Internal hemorrhoids may prolapse or bleed, but rarely turn into painful except they develop thrombosis and necrosis (usually related to extreme prolapse, incarceration, and/or strangulation). Firstdegree hemorrhoids bulge into the anal canal and will prolapse past the dentate line on straining. Third-degree hemorrhoids prolapse through the anal canal and require guide discount. Combined internal and exterior hemorrhoids straddle the dentate line and have traits of each inner and exterior hemorrhoids. Postpartum hemorrhoids outcome from straining throughout labor, which leads to edema, thrombosis, and/or strangulation. Hemorrhoidectomy is often the treatment of choice, particularly if the affected person has had chronic hemorrhoidal signs. Portal hypertension was lengthy thought to enhance the chance of hemorrhoidal bleeding due to the anastomoses between the portal venous system (middle and higher hemorrhoidal plexuses) and the systemic venous system (inferior rectal plexuses).
Syndromes
- Broken bone
- Meconium is made in the intestinal tract.
- Loss of vision
- Childbirth
- Congestive heart failure
- The amount swallowed
- Chest x-ray - may also show fluid in the lungs or prominent lung veins
- Coos
- If your cholesterol is high, eat a low-cholesterol and low-fat diet.
10 mg zetia generic with amex
Bowel continuity is restored by anastomosis of an ileal reservoir to the anal canal cholesterol yahoo zetia 10 mg low cost. The original approach included a transanal mucosectomy and hand-sewn ileoanal anastomosis cholesterol synthesis definition buy zetia 10 mg low price. Proponents of this technique argue that mucosectomy ensures removing of all the diseased mucosa, together with the anal transition zone, and therefore decreases the danger of ongoing disease, dysplasia, and carcinoma. The neorectum is made by anastomosis of the terminal ileum aligned in a "J," "S," or "W" configuration. Because practical outcomes are comparable and because the J-pouch is the best to assemble, it has turn into the most used configuration. With growing experience in laparoscopic and robotic colectomy, some facilities have begun performing complete proctocolectomy with ileal pouch�anal reconstruction utilizing minimally invasive surgical techniques. The ileostomy is then closed 6 to 12 weeks later, after a contrast study confirms the integrity of the pouch. In low-risk sufferers, nonetheless, there are stories of successful creation of an ileoanal pouch without a diverting stoma. After a complete colectomy and resection of the rectum (A), the anal canal with a brief cuff of transitional mucosa and sphincter muscle tissue is preserved (B). An ileal J-pouch has been constructed and is anastomosed to the anal canal using a double-staple method (C). A high anterior resection is the time period used to describe resection of the distal sigmoid colon and upper rectum and is the suitable operation for benign lesions and illness on the rectosigmoid junction similar to diverticulitis. The inferior mesenteric artery is ligated at its base, and the inferior mesenteric vein, which follows a unique course than the artery, is ligated separately. A primary anastomosis (usually end-to-end) between the colon and rectal stump with a short cuff of peritoneum surrounding its anterior two thirds usually can be performed. The rectosigmoid is mobilized, the pelvic peritoneum is opened, and the inferior mesenteric artery is ligated and divided both at its origin from the aorta or simply distal to the takeoff of the left colic artery. The rectum is mobilized from the sacrum by sharp dissection beneath direct view throughout the endopelvic fascial airplane. The dissection could additionally be carried out distally to the anorectal ring, extending posteriorly by way of the rectosacral fascia to the coccyx and Because the chance of an anastomotic leak and subsequent sepsis is greater when an anastomosis is created in the distal rectum or anal canal, creation of a temporary ileostomy ought to be thought of on this setting. Although an anastomosis may be technically feasible very low in the rectum or anal canal, it is essential to note that postoperative perform may be poor. Because the descending colon lacks the distensibility of the rectum, the reservoir function could also be compromised. Pelvic radiation, prior anorectal surgical procedure, and obstetrical trauma could trigger unsuspected sphincter damage. Creation of a colon J-pouch or transverse coloplasty might improve operate, however few long-term research have addressed this concern. The term is typically used when the left or sigmoid colon is resected and the closed off rectum is left within the pelvis. If the distal colon is long sufficient to reach the belly wall, a mucus fistula may be created by opening the defunctioned bowel and suturing the open lumen to the skin. The abdominal-pelvic portion of this operation proceeds in the same trend as described for an extended low anterior resection. The perineal dissection can be carried out with the patient in lithotomy place (often by a second surgeon) or within the prone position after closure of the stomach and creation of the colostomy. For most cancers, the perineal dissection is designed to excise the anal canal with a large circumferential margin including a cylindrical cuff of the levator muscle. Primary wound closure is usually profitable, however a large perineal defect, particularly if preoperative radiation has been used, could require a vascularized flap closure in some patients. For benign disease, proctectomy may be carried out utilizing an intersphincteric dissection between the interior and exterior sphincters. This method minimizes the perineal wound, making it easier to close as a outcome of the levator muscle stays intact. The rectum and accompanying mesorectum are divided at the acceptable degree, relying on the character of the lesion. A low rectal anastomosis normally requires mobilization of the splenic flexure and ligation and division of the inferior mesenteric vein simply inferior to the pancreas. Circular stapling gadgets have tremendously facilitated the conduct and improved the protection of the colon to extraperitoneal rectal anastomosis. An extended low anterior resection is critical to remove lesions situated in the distal rectum, however a number of centimeters above the sphincter. The rectum is totally mobilized to the extent of the levator ani muscle just as for a low anterior resection, but the anterior dissection is extended alongside the rectovaginal septum in girls and distal to the seminal vesicles and prostate in men. After resection at this stage, a coloanal anastomosis can be created utilizing one of a wide range of methods. An end-to-end stapled or hand-sewn anastomosis has historically been the procedure of choice. However, the practical consequences of a "straight" anastomosis have led to consideration for creation of a colon J-pouch or transverse coloplasty to improve the capability of the neorectal reservoir. The geometry of the anastomosis could also be end-to-end, end-to-side, side-to-end, or side-to-side. The submucosal layer of the intestine provides the strength of the bowel wall and must be integrated in the anastomosis to assure therapeutic. The alternative of anastomosis depends on the operative anatomy and surgeon desire. Although many surgeons advocate one method over another, none has been confirmed to be superior. Accurate approximation of two well-vascularized, healthy limbs of bowel without pressure in a normotensive, wellnourished patient almost always results in a great outcome. An end-to-end anastomosis can be performed when two segments of bowel are roughly the same caliber. This method is most often employed in rectal resections, however may be used for colocolostomy or small bowel anastomoses. An end-to-side configuration is beneficial when one limb of bowel is bigger than the other. A side-to-end anastomosis is used when the proximal bowel is of smaller caliber than the distal bowel. A side-to-end anastomosis might have a much less tenuous blood supply than an end-to-end anastomosis. A side-to-side anastomosis permits a big, wellvascularized connection to be created on the antimesenteric facet of two segments of intestine. Any of the configurations described earlier may be created utilizing a hand-sutured or stapled method. Hand-sutured anastomoses could also be single layer, using both working or interrupted stitches, or double layer.
10 mg zetia buy mastercard
The subsequent unequal progress of the lateral wall of the cecum causes the appendix to discover its grownup position on the posterior medial wall cholesterol food sources buy zetia 10 mg visa, just below the ileocecal valve test your cholesterol with a simple photo buy zetia 10 mg without a prescription. The base of the appendix may be located by following the longitudinally oriented taeniae coli to their confluence on the cecum. The tip of the appendix could be situated anywhere in the best decrease quadrant of the abdomen, pelvis, or retroperitoneum. With midgut malrotation, the midgut (small bowel and proximal colon) incompletely rotates or fails to rotate around the axis of the superior mesenteric artery throughout fetal improvement. In this situation, the appendix will remain within the left upper quadrant of the abdomen. Situs inversus is a uncommon autosomal recessive congenital defect characterised by the transposition of belly and/or thoracic organs. In this case, the appendix is discovered in the left decrease quadrant of the abdomen. The outer diameter varies between 3 and 8 mm, whereas the luminal diameter varies between 1 and three mm. This artery originates pos- Anatomy terior to the terminal ileum, entering the mesoappendix close to the bottom of the appendix. Innervation of the appendix is derived from sympathetic elements contributed by the superior mesenteric plexus (T10-L1) and afferents from the parasympathetic elements through the vagus nerves. Lymphoid aggregates occur within the submucosal layer and should lengthen into the muscularis mucosa. The mucosa is like that of the large gut, aside from the density of the lymphoid follicles. The crypts are irregularly sized and formed, in contrast to the extra uniform appearance of the crypts in the colon. Neuroendocrine complexes composed of ganglion cells, Schwann cells, neural fibers, and neurosecretory cells are positioned slightly below the crypts. It is now nicely recognized that the appendix is an immunologic organ that actively participates in the secretion of immunoglobulins, significantly immunoglobulin A. However, this association is only seen in sufferers handled with appendectomy for appendicitis before age 20. The appendix could operate as a reservoir to recolonize the colon with wholesome micro organism. One retrospective examine demonstrated that prior appendectomy might have an inverse relationship to recurrent Clostridium difficile infections. The mucosa of the appendix is susceptible to impairment of blood supply; thus, its integrity is compromised early in the process, which allows bacterial invasion. The space with the poorest blood supply suffers essentially the most: ellipsoidal infarcts develop within the antimesenteric border. As distension, bacterial invasion, compromise of the vascular provide, and infarction progress, perforation happens, normally on the antimesenteric border simply past the point of obstruction. However, an association with numerous contagious micro organism and viruses has solely been present in a small proportion of appendicitis patients. About 60% of aspirates of inflamed appendices have anaerobes in comparability with 25% of aspirates from regular appendices. Patients with gangrene or perforated appendicitis seem to have extra tissue invasion by Bacteroides. Because of the current predilection for surgical therapy, the pure historical past of appendicitis has not been nicely described. An increasing quantity of circumstantial proof means that not all patients with appendicitis will progress to perforation and that decision may be a typical occasion. These research discovered three to five instances more patients with appendicitis within the group of sufferers who had been randomized to laparoscopy. In the United States, it reached its lowest incidence fee of about 15 per 10,000 inhabitants within the 1990s. Obstruction of the lumen as a end result of fecaliths or hypertrophy of lymphoid tissue is proposed as the principle etiologic factor in acute appendicitis. Fecaliths and calculi are present in 40% of cases of simple acute appendicitis,23 in 65% of instances of gangrenous appendicitis without rupture, and in practically 90% of cases of gangrenous appendicitis with rupture. The proximal obstruction of the appendiceal lumen produces a closed-loop obstruction, and persevering with regular secretion by the appendiceal mucosa rapidly produces distension. Distension of the appendix stimulates the nerve endings of visceral afferent stretch fibers, producing obscure, dull, diffuse ache within the mid-abdomen or lower epigastrium. Distension will increase from continued mucosal secretion and from fast multiplication of the resident bacteria of the appendix. Capillaries and venules are occluded however arterial influx continues, leading to engorgement and vascular congestion. The inflammatory Epidemiology Natural History Etiology and Pathogenesis Clinical Presentation the inflammatory course of in the appendix presents as ache, which initially is of a diffuse visceral sort and later becomes more localized because the peritoneal lining will get irritated Table 30-1). Appendicitis normally starts with periumbilical and diffuse ache that eventually localizes to the right lower quadrant (sensitivity, 81%; specificity, 53%). Variations within the anatomic location of the appendix could account for the differing shows of the somatic part of ache. Gastrointestinal symptoms that develop before the onset of pain counsel a unique etiology similar to gastroenteritis. Changes of larger magnitude may point out that a complication has occurred or that another analysis must be thought-about. Patients with appendicitis often transfer slowly and like to lie supine due to the peritoneal irritation. When the pressure of the examining hand is shortly relieved, the affected person feels a sudden pain, the so-called rebound tenderness. It is subsequently beneficial to start with testing for indirect rebound tenderness and direct percussion tenderness. Anatomic variations within the place of the inflamed appendix lead to deviations within the usual bodily findings. With a retrocecal appendix, the abdominal findings are much less putting, and tenderness could additionally be most marked in the flank. When the appendix hangs into the pelvis, stomach findings may be completely absent, and the analysis may be missed. Right-sided rectal tenderness is said to help in this scenario, however the diagnostic value is low. Pain with extension of the proper leg (psoas sign) signifies a focus of irritation in the proximity of the proper psoas muscle. Similarly, stretching of the obturator internus via inner rotation of a flexed thigh (obturator sign) suggests inflammation near the muscle.
Zetia 10 mg discount visa
As anticipated cholesterol in cage free eggs generic zetia 10 mg free shipping, the secondary intervention rate was greater within the endoluminal group (9 cholesterol levels 60 year old 10 mg zetia safe. Patients needed to be eligible for both sort of restore so as to be included in the research. Six aneurysm ruptures were confirmed in the endovascular repair group versus none in the open restore group. Endovascular restore led to elevated long-term survival among youthful patients however not amongst older sufferers, for whom a higher benefit from the endovascular strategy had been expected. Matsumura and associates compared endoluminal versus open restore using the Excluder gadget. The Zenith system by Cook has been studied by Greenberg and associates, who in contrast standard surgical repair with endoluminal repair in low-risk patients and endoluminal repair in high-risk patients. Interestingly, short-neck patients (<15 mm) had no aneurysm growths and a 2% migration price. The current climate of value containment and limited reimbursement for healthcare providers mandates a critical evaluation of the economic impact of any new medical expertise on the market. The in-hospital prices for both endovascular and open repair embody graft value, operating room fees, radiology, pharmacy, ancillary care, intensive care unit charges, and floor expenses. Despite the improved morbidity and mortality charges, a number of early research have reported no cost profit with the application of endovascular repair. Despite commercialization of endovascular repair, the gadget costs are still within the vary of $5000 to $6000 with no indicators of abating. There were no differences present in survival, quality of life, and costs after 2 years between the endovascular and the open group. Costs remained decrease after 2 years in the endovascular group, but the distinction was no longer significant. A computed tomography scan demonstrating an endoleak (small arrow) as evidenced in contrast flow outdoors the aortic endograft (long arrow). Type I endoleak refers to fixation-related leaks that happen on the proximal or distal attachment websites. These represent less than 5% of all endoleaks and are seen as an early blush of contrast into the aneurysm sac from the proximal or distal ends of the device throughout completion angiography. They are the most typical kind of endoleak, accounting for 20% to 30% of all instances, and about half resolve spontaneously. Multiple massive series have reported that an annual rupture rate of roughly 1% to 1. It has been shown that even successfully excluded aneurysms can result in the event of attachment-site leaks and device failure, caused in part by aneurysm remodeling resulting in stent migration or kinking. May and associates reported a mortality rate of 43% in these sufferers who underwent open conversion. Several stories have proven that endovascular restore could be performed successfully in patients beforehand handled with endoluminal prostheses. Autopsy studies have demonstrated splanchnic atherosclerosis in 35% to 70% of circumstances. On the opposite hand, mesenteric ischemia can occur abruptly, as within the case of thromboembolism. Despite recent progress in perioperative management and higher understanding of pathophysiology, mesenteric ischemia is considered one of the catastrophic vascular issues with mortality charges starting from 50% to 75%. In roughly 5% of instances after an apparently profitable endovascular restore, the aneurysm continues to develop without any demonstrable endoleak. Although it was initially thought that an endoleak was actually present but simply not detected, case have been reported the place the aneurysm has been surgically opened and the contents have been completely devoid of any blood and no extravasation might be discovered. The mechanism of continued pressurization of the aneurysm sac following profitable exclusion from the arterial circulation stays unsolved presently. Conservatively talking, until further long-term data become obtainable, if the affected person is a suitable surgical threat, elective open conversion should be considered. It is estimated that mesenteric ischemia accounts for 1 in each 1000 hospital admissions on this nation. The prevalence is rising due partly to the elevated consciousness of this illness, the superior age of the population, and the significant comorbidity of these aged sufferers. Early recognition and prompt treatment earlier than the onset of irreversible intestinal ischemia are essential to improve the outcome. These anatomic origins in relation to the aorta are essential when a mesenteric angiogram is performed to determine the luminal patency. Because of the ample collateral circulate between these mesenteric arteries, progressive diminution of flow in a single or even two of the primary mesenteric trunks is normally tolerated, provided that uninvolved mesenteric branches can enlarge over time to provide enough compensatory collateral circulate. In distinction, acute occlusion of a major mesenteric trunk may lead to profound ischemia because of lack of sufficient collateral circulate. Regulation of mesenteric blood circulate is largely modulated by both hormonal and neural stimuli, which characteristically regulate systemic blood circulate. In addition, the mesenteric circulation responds to the gastrointestinal contents. Hormonal regulation is mediated by splanchnic vasodilators, such as nitric oxide, glucagon, and vasoactive intestinal peptide. Certain intrinsic vasoconstrictors, such as vasopressin, can diminish the mesenteric blood move. On the opposite hand, neural regulation is supplied by the intensive visceral autonomic innervation. Injured bowel mucosa allows unimpeded inflow of toxic substances from the bowel lumen with systemic penalties. If full-thickness necrosis happens within the bowel wall, intestinal perforation ensues, which is in a position to lead to peritonitis. Concomitant atherosclerotic illness in cardiac or systemic circulation incessantly compounds the diagnostic and therapeutic complexity of mesenteric ischemia. Types of Mesenteric Artery Occlusive Disease There are three main mechanisms of visceral ischemia involving the mesenteric arteries: (a) acute mesenteric ischemia, which could be both embolic or thrombotic in origin; (b) chronic mesenteric ischemia; and (c) nonocclusive mesenteric ischemia. Despite the variability of these syndromes, a typical anatomic pathology is concerned in these processes. Acute thrombosis happens in patients with underlying mesenteric atherosclerosis, which typically includes the origin of the mesenteric arteries while sparing the collateral branches. Nonocclusive mesenteric ischemia is characterised by a low move state in in any other case normal mesenteric arteries and most regularly occurs in critically unwell sufferers on vasopressors. Finally, continual mesenteric ischemia is a practical consequence of a long-standing atherosclerotic process that typically includes no less than two of the three major mesenteric vessels. An anteroposterior view of a selective superior mesenteric artery angiogram exhibits an abrupt cutoff of the middle colic artery, which was caused by emboli (arrow) due to atrial fibrillation. Several much less frequent syndromes of visceral ischemia involving the mesenteric arteries can also cause critical debilitation. Chronic mesenteric ischemic symptoms can happen because of extrinsic compression of the celiac artery by the diaphragm, which is termed median arcuate ligament syndrome or celiac artery compression syndrome.