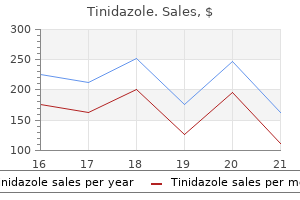
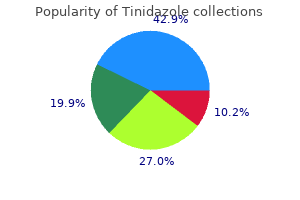
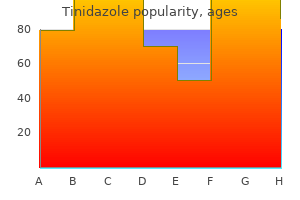
Tinidazole dosages: 1000 mg, 500 mg, 300 mg
Tinidazole packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Discount tinidazole 1000 mg amex
Because of the potential for hemorrhage broad spectrum antibiotics for sinus infection cheap tinidazole 300 mg otc, it is suggested that discount be attempted in the working room underneath general anesthesia with consciousness by a thoracic or a vascular surgeon termin 8 antimicrobial preservative purchase tinidazole 1000 mg line. Some advocate that a thoracic surgeon be scrubbed in on the time of discount (8), particularly for circumstances with delayed therapy (>1 week) because the medial finish of the clavicle could also be adherent to adjoining vascular structures. Fractures with anterior or superior displacement are often managed nonoperatively. Closed discount is attempted in acute accidents by longitudinal traction, abduction, and shoulder extension of the concerned arm and is often profitable. In posteriorly displaced dislocations, the reduction could be unstable due to the posteriorly directed Medial Clavicle Fracture and Sternoclavicular Separation. Therefore, displacements of the medial finish of the clavicle are normally physeal separations that mimic sternoclavicular dislocation (7). Posterior displacement by fracture or dislocation may cause dysphagia or respiratory compromise. Physical examination and plain radiography are unreliable in assessing displacement. These accidents are incessantly missed, and a excessive index of suspicion for sternoclavicular injury is required in patients with ache and tenderness in the area. Posteriorly displaced medial clavicle fractures or sternoclavicular dislocations are often treated operatively to relieve compression of mediastinal buildings. If the surgeon believes a secure discount is achieved, postoperative axial imaging should be obtained to document maintenance of reduction. If the discount is unstable, or with late presentation, open reduction and fixation is performed. The surgical preparation extends from the midneck to abdomen, and throughout the chest to embrace the contralateral acromioclavicular joint. Having a thoracic or vascular surgeon on standby and emergency thoracotomy devices available is beneficial (8, 9, 19) the ipsilateral upper extremity can be prepped into the surgical subject if desired to allow traction through the arm and stability testing with vary of motion of the shoulder after fixation. The medial clavicle is approached via a transverse incision extending from the center thirdέedial third junction of the clavicle to just previous the midpoint of the sternal notch. Subcutaneous dissection is performed by way of the platysma to the extent of the periosteum, and then the periosteum is incised from lateral to medial instantly anterior over the clavicle. As the dissection proceeds medially, the periosteum will stay intact and hooked up to the medial clavicular epiphysis in physeal accidents and should be preserved. In dislocations, the periosteum will typically be hooked up anteriorly to the fibrocartilaginous disc of the sternoclavicular joint. Instead, cautious subperiosteal circumferential dissection across the clavicle close to the middle thirdέedial third junction could be carried out, and a clamp can then be placed around the clavicle extra laterally. This will assist in stabilizing the clavicle for cautious subperiosteal dissection with an elevator working from lateral to medial. During reduction of dislocations, you will want to understand that only in regards to the inferior one-third to one-half of the medial clavicle articulates with the sternal notch. Intraoperative photograph (with head to left) of blunt-tip clamp round medial right clavicle. The metaphysis is displaced posteriorly and cephalad from the epiphysis, which is visible between the two Senn rake retractors. Suture fixation, wire fixation, and tendon weave through bone tunnels have all been recommended. For physeal accidents, suture or sternal wire fixation from the metaphysis to the epiphysis (medial clavicular head) is sufficient. For dislocations, drill holes through sternum are used with figure-of-eight heavy suture to the anterior medial clavicle. After restore, the adequacy of discount and stability are assessed underneath direct visualization. The stability is examined by direct posterior pressure (and range of motion of the ipsilateral shoulder if desired). The periosteum is often thick and is then closed over the clavicle to increase the fixation. The affected person is positioned in a sling for 4 weeks, and for six weeks the affected person avoids crossarm adduction and heavy lifting with the concerned extremity. The mechanism of harm to the distal clavicle is just like adult acromioclavicular separation. This is as a end result of the distal epiphysis of the clavicle stays a cartilaginous cap until the age of 20 years or older (6), whereas the acromioclavicular and coracoclavicular ligaments are firmly hooked up to the thick periosteum of the clavicle. Because these injuries represent physeal disruption with herniation of bone from the periosteal tube, super potential for therapeutic and reworking exists. Lifting the clamp on medial clavicle anteriorly reduces the metaphysis to the epiphysis (beneath Senn rake retractor) prior to figure-of-eight suture fixation. A sling or shoulder immobilizer is used for 3 weeks, adopted by a graduated exercise program. Even in aggressive athletes, shoulder strength and vary of movement are usually not impaired after rehabilitation (17ͱ9). The occasional patient who develops late signs of pain and stiffness could additionally be relieved by resection of the distal clavicle (18), with ligament reconstruction. In grade V separations, the clavicle is displaced 100 percent to 300% superiorly, and the clavicle lies subcutaneously. Therefore, preliminary analysis should embody a diligent search for more critical chest accidents, similar to rib fractures, pulmonary or cardiac contusion, and harm to the mediastinum. If associated with accidents to the clavicle, scapulothoracic dissociation ought to be suspected, and a careful evaluation of the vascular and neurologic perform of the ipsilateral higher extremity must be carried out. Avulsion fractures of the scapula have additionally been reported and are a results of indirect trauma (20). Treatment of most scapular fractures consists of immobilization with a sling and swathe, followed by early shoulder motion after pain has subsided. The scapular body is encased in thick muscle tissue, so displacement is rare and well tolerated after therapeutic (12). Fractures of the acromion or coracoid require surgery only when severely displaced. Intra-articular fractures with substantial displacement should be restored to anatomic positions. Large glenoid rim fractures may be related to Metaphysis Treatment of most distal clavicle fractures consists of support with a sling or shoulder immobilizer for three weeks. Reduction and fixation are pointless, except for the rare occasion in which the clavicle is severely displaced in an older adolescent (12). Fracture or physeal separation of the distal clavicle is more common, and has been called pseudodislocation of the acromioclavicular joint (13). Tenderness over the acromioclavicular joint and prominence of the lateral end of the clavicle are current with fracture, physeal separation, and joint separation. Radiographs reveal increased distance between the coracoid course of and the clavicle, compared with the other aspect. When true joint separation occurs, the damage could also be a sprain, subluxation, or dislocation.
1000 mg tinidazole order with amex
The sharp Hohmann is once more impacted to assist in retraction of the psoas and neurovascular bundles k. pneumoniae antibiotic resistance tinidazole 500 mg best. Medial to the iliopectineal eminence antibiotics mechanism of action tinidazole 1000 mg buy online, the superior pubic ramus is dissected in a subperiosteal fashion and curved Lane retractors are positioned into the obturator foramen across the ramus. A straight osteotome is then used to perform the osteotomy with the retractors offering soft-tissue safety. The osteotomy begins medial to the iliopectineal eminence and is angled roughly forty five levels from anterolateral to posteromedial, in addition to being angled from distalάateral to proximalέedial. The osteotomy can sometimes be incomplete posteriorly, which will significantly impede fragment rotation later; consequently, ensuring that the osteotomy is complete at this point is essential. Performing this osteotomy with a Gigli saw passed by way of the obturator foramen is another method. If an arthrotomy of the hip is to be carried out, it must be accomplished at this level. The femoral head, labrum, and rim can be inspected and any intraarticular pathology treated. The capsule can be closed at this level or left open to permit direct visualization to rule out impingement after acetabular rotation has taken place. At this point, the deep medial dissection of the pelvis is continued over the pelvic brim toward the ischial spine, utterly releasing the quadrilateral plate. A narrow-spiked Hohmann retractor is positioned gently inside the tunnel to shield the abductors through the ensuing iliac osteotomy made with the oscillating noticed. The posterior column osteotomy is performed with the hip almost fully prolonged, to relax the nearby sciatic nerve. It is made with a straight chisel, starting on the medial surface of the ilium, at the posterior end of the noticed reduce. This osteotomy is directed on the ischial backbone, at an angle of about 120 levels with the iliac saw reduce. Image intensifier control within the fake profil projection allows visualization of the gap of this osteotomy line from the acetabulum because it bisects the posterior column between the posterior acetabulum and the sciatic notch (see inset). After the medial cortex is split to a point a minimal of 4 cm beneath the iliopectineal line, the proximal lateral cortex could be rigorously divided with a chisel, as a bone spreader distracts the iliac osteotomy, stressing the remaining bone bridges. The remaining deep medial bone bridge is usually not extra than about 2 cm in length. Using a T-handle chuck and lamina spreaders via the anterior portion of the iliac osteotomy, the remaining bone bridge will fracture. It is important to be sure that the chisel is at least 4 cm beneath the pelvic brim so as to avoid an intraarticular osteotomy. The usual correction maneuver includes anterior rotation of the acetabulum within the axis of the ilium, which improves each anterior and lateral coverage. Occasionally, lateral rotation is required as well, as is medial rotation to keep away from retroversion. After the specified quantity of correction is achieved, two or three provisional k-wires are positioned through the iliac crest into the acetabular fragment. A plain anteroposterior radiograph is then taken to verify correct fragment positioning. It is essential to assess not solely that the weight-bearing zone is horizontal or near-horizontal but also the congruity of the hip joint, the model of the acetabulum, the extent of medialization or lateralization, and Shenton line. The capsulotomy is closed at this level, if it has not already been closed, and the fragment is secured with a minimal of three screws. The straight head of the rectus is secured through the outlet left by the Schanz screw, giving a strong transosseous restore. The periosteum and stomach wall musculature is secured through drill holes to the iliac crest. This 15-year-old feminine figure skater offered with a 1-year history of progressive anterolateral left hip pain. A: Anteroposterior, faux profil, and von Rosen views show left hip dysplasia with decreased anterior and lateral center-edge angles and an upsloping sourcil. The rim fracture has healed, anterior and lateral center-edge angles have improved, the sourcil is horizontal, and her symptoms have resolved. There has been significant confusion within the literature as to what particularly is a Dega osteotomy. Whereas the Pemberton osteotomy ends within the ilioischial limb of the triradiate cartilage and utterly divides the iliac bone from anterior to this point, the Dega osteotomy ends just above the horizontal portion of the triradiate cartilage (the ilioischial and iliopubic portions) and leaves a posterior portion of each the inner and outer iliac cortex simply anterior to the sciatic notch intact, forming its hinge. After the iliac apophysis is split, the inner and outer tables of the ilium are uncovered subperiosteally, which is enough to expose the sciatic notch on each side. If more anterior coverage is desired (A), the airplane of the osteotomy is more transverse. If lateral protection is desired (B), the aircraft of the osteotomy is inclined more laterally. After that is determined (C), a small, osteotome can be utilized to define the osteotomy by slicing the cortex of the inside and outer desk. The osteotomy is begun about 1 cm above the anteroinferior iliac backbone and proceeds posteriorly, keeping about 1 to 1. Care in exposing the sciatic notch as far inferiorly as attainable makes this error easier to avoid by seeing the portion of the ilium that lies between the sciatic notch posteriorly and the capsule of the hip joint anteriorly. It is neither attainable, essential, nor advisable, nevertheless, to expose this right down to the triradiate cartilage. The similar downside exists when cutting the cortex of the inside table, but to not the same extent. By twisting it, the tissue is retracted, giving good exposure to the posterior area distal to the sciatic notch where visualization is most difficult. After the inner and outer cortices of the ilium are divided as far as can be seen, a wider curved osteotome is used to join these two cuts. At this level, an osteotome with a right-angled curve is inserted into the osteotomy. This could be made simpler by prying down on the acetabular roof with an osteotome and inserting a small lamina spreader to hold the osteotomy aside. When the osteotomy is full, the acetabular roof may be levered down into the desired place and held there with a lamina spreader. Grooves are prepared within the cancellous floor on both sides of the osteotomy to present safe fixation of the bone graft. When femoral shortening accompanies the procedure, the resected femur may be used as the supply of the bone graft. When in place, the bone graft must be safe and secure, and this might be verified by making an attempt to dislodge the graft. A radiograph instantly after surgery (A) demonstrates the osteotomy extending into the triradiate cartilage and never breaking into the sciatic notch. Radiographs at 6 weeks (B) and 6 months (C) reveal the rapid healing and the superb coverage of the femoral head. The positioning and exposure for the Dega osteotomy are the identical as for the other pelvic osteotomies.
Generic tinidazole 1000 mg online
Although a medial parapatellar incision makes it barely easier to attain the semitendinosus tendon bacteria have dna tinidazole 500 mg buy free shipping, a long midline incision how do antibiotics for acne work generic tinidazole 300 mg with visa, as described for proximal realignment, is healthier cosmetically. The semitendinosus is the most posterior, behind the knee, and is the deepest or most posterior tendon inserting into the tibia. The infrapatellar department of the saphenous nerve can normally be observed emerging from the Sartorius. Although a few of its sensory twigs may be divided, care ought to be taken with this nerve to keep away from a large area of anesthesia (B). With the knee flexed, the pores and skin flap is retracted with an extended blade retractor and blunt dissection is continued posteriorly and proximally (A). Next, the tendon must be followed to its insertion posterior to the Sartorius and gracilis tendons, releasing all extraneous attachments with care to avoid chopping the saphenous nerve (B). A complete lateral launch should be carried out, at the minimum, including each the capsule and the synovium. At this point, the surgeon can determine whether or not to perform a more intensive realignment of the patella with advancement of the vastus medialis muscle or an entire proximal realignment. If nothing more is to be carried out (as illustrated here for simplicity), a small incision ought to be made within the medial capsule on the distal end of the patella. This will permit palpation of the inferior floor of the patella for more accurate placement of the drill gap. With the patella held within the desired position and the tendon pulled throughout the floor of the patella, the right course for the drill gap can be determined (A). Starting at the inferior medial fringe of the patella, a gap of enough measurement to allow passage of the tendon is drilled, emerging on the superior lateral nook of the patella (B). In directing the drill, the surgeon must be cautious to keep away from penetrating the articular surface. Sufficient pressure should be positioned on the tendon to maintain the patella according to the intercondylar notch. This can be examined by flexing the knee whereas an assistant holds pressure on the tendon. Note the infrapatellar department of the saphenous nerve that penetrates the Sartorius muscle and branches over the medial capsule of the knee. The major department of the saphenous nerve emerges from between the Sartorius and gracilis tendons to continue down the leg. Care should be taken throughout each the dissection and the routing of the tendon to be certain that these nerve are neither blocked nor kinked. The operation is completed by suturing the semitendinosus tendon to the periosteum of the patella and, if sufficient length is on the market, to itself. To restore rigidity to the patellar tendon and effect some redirection in its line of pull, a Goldthwait process may be added. This entails splitting the patellar tendon in half, detaching the lateral half, directing this half beneath the medial half of the tendon, and attaching it to the periosteum of the tibia underneath reasonable rigidity. At the completion of this step, any muscle developments or other steps to increase the realignment are accomplished, and the wound is closed over a suction drain. Semitendinosus Tenodesis of Patella for Recurrent Dislocation: the Galeazzi Procedure. The Galeazzi procedure transfers the semitendinosus to the inferior pole of the patella. From there, it courses through a drill hole positioned obliquely by way of the patella, exiting the superior lateral facet. This offers a medial tether and effectively alters the net vector of the patellar tendon towards the medial side. Typically, the vastus medialis is superior roughly one-third the width of the patella. C: the Fulkerson modification involves an oblique cut that ends in anterior translation as the tubercle is moved medially. This reduces the patellofemoral contact forces while shifting the pull of the patella medially. This is now my preferred technique of surgical management of the adolescent with recurrent patellar dislocation. If the Q angle is extreme, distal realignment is performed; the Roux-Goldthwait procedure is used for the skeletally immature patients up to 14 years of age and the Elmslie-Trillat procedure for patients older than 14 years. The larger therapeutic potential of the pediatric meniscus and the results of meniscectomy in a young lively affected person (increased contact forces and early osteoarthritic changes) underscore the importance of proper analysis and treatment of pediatric meniscal accidents. New surgical strategies have facilitated arthroscopic meniscal repair which has become the standard of look after repairable tears. The lateral half is transferred beneath the medial facet and sutured to the periosteum along the metaphysis. Acceptable outcomes may be expected in as much as 90% of cases using the Roux-Goldthwait procedure. An option is to sharply dissect the entire patellar tendon from its insertion utilizing a scalpel and to resuture it more medially to restore a traditional Q angle (62). Care have to be taken not to move the insertion too distally, which may lead to patella baja and significant pain. It is essential to move the knee early, and immobilization in a removable knee immobilizer for 3 to 4 weeks is adequate for therapeutic. Active vary of movement and strengthening are important components of the rehabilitation program, and a resumption of sports activity may be anticipated in 4 to 6 months. These prevent the medial meniscus from translating greater than 2 to 5 mm with knee motion. The round lateral meniscus covers 70% of the lateral tibial plateau and lacks attachments to the fibular collateral ligament and at the popliteus hiatus. This ends in elevated mobility of the lateral meniscus, which usually translates 9 to 11 mm throughout knee motion. Meniscal blood provide arises from the geniculate arteries which type a peripheral perimeniscal synovial plexus. The creating meniscus is totally vascularized at birth, and its vascularity steadily diminishes to the peripheral 10% to 30% of the meniscus (red-red zone) by age 10 at which era it resembles the grownup meniscus (64, 65). Synovial diffusion is responsible for diet of the central portion of the meniscus. The menisci are load sharing and scale back contact stresses throughout the knee joint, transmitting 50% to 70% of the load in extension and 85% of the load in ninety levels of flexion (66). Nondiscoid meniscal tears normally happen in older children following a twisting knee injury (65, 67Ͷ9). Meniscal injuries in children generally present with joint line pain and swelling. The bodily examination by experienced examiners reliably diagnoses medial (62% sensitivity, 80% specificity) and lateral (50% sensitivity, 89% specificity) meniscal tears in kids (70).
Purchase tinidazole 500 mg on-line
Construction of a knee joint in congenital complete absence of the tibia (paraxial hemimelia tibia) global antibiotic resistance journal 500 mg tinidazole buy with amex. Failure of centralization of the fibula for congenital longitudinal deficiency of the tibia antimicrobial incise drape buy cheap tinidazole 1000 mg online. Congenital diastasis of the inferior tibiofibular joint: a review of the literature and report of two cases. Wedge-shaped distal tibial epiphysis within the pathogenesis of equinovalgus deformity of the foot and ankle in tibial lengthening for fibular hemimelia. Natural historical past and treatment of instability of the hip in proximal femoral focal deficiency. Growth patterns after lengthening of congenitally short lower limbs in young youngsters. Complex congenital anomalies of the decrease extremities: femoral bifurcation, tibial hemimelia, and diastasis of the ankle. Treatment of longitudinal deficiency affecting the femur: evaluating patient mobility and satisfaction outcomes of Syme amputation against extension prosthesis. Rotation-plasty for congenital defects of the femur: making use of the ankle of the shortened limb to control the knee joint of a prosthesis. Van Nes rotational osteotomy for therapy of proximal femoral focal deficiency and congenital brief femur. Quality of life in survivors with a van Ness-Borggreve rotationplasty after bone tumour resection. Malignant tumor of the distal a part of the femur of the proximal a half of the tibia: endoprosthetic alternative of rotationplasty. Morphologic characteristics of acetabular dysplasia in proximal femoral focal deficiency. Early conservative and operative treatment to achieve early normal development in proximal femoral focal deficiency. Resection, rotationplasty, and femoropelvic arthrodesis in extreme congenital femoral deficiency. Impact of prostheses on function and quality of life for youngsters with unilateral congenital belowthe-elbow deficiency. Prosthetic units for children with bilateral upper limb deficiencies: when and if, execs and cons. A long-term review of kids with congenital and purchased upper limb deficiency. The Krukenberg process: a surgical possibility for the therapy of double hand amputees in Sierra Leone. The value of the Krukenberg operation and its indication despite trendy prosthesis of the hand. Lengthening of congenital below-elbow amputation stumps by the Ilizarov approach. Does socket configuration influence the position of the femur in above-knee amputation? The influence of four-bar linkage knees on prosthetic swing-phase floor clearance. Gait analysis and vitality value of below knee amputees carrying six totally different prosthetic feet. Comparison of energy price and gait effectivity during ambulation in below-knee amputees using totally different prosthetic toes - a preliminary report. It is estimated that approximately 30 million children and youth between the ages of 6 and 21 years engage in sports activities applications which may be held outdoors of faculty, and seven. Parents want to know if the benefits of the sports activities actions warrant the risks concerned, so an understanding of sportsspecific dangers is essential to provide a comprehensive approach to tackle this concern. With applicable surveillance studies of each sport, particular risks and patterns of damage associated with totally different sports could be decided and compared. From this information, it may be attainable to develop specific interventions designed to scale back the frequency of injuries. First, there are sport-specific information that establish the chance of harm to participants for most sports (2͵). The figures for kids and youth in 2008 reveal that injuries occurred most regularly in football, adopted by basketball, soccer, and baseball and that over 2 million youngsters under age 18 required medical attention for injuries (2) (Table 31-1). Research examined data submitted by athletic trainers at a hundred high colleges within the United States. Severe injuries occurred in approximately 15% of all sports-related accidents and had been defined as lack of participation in sports activities of no much less than 21 days. Injuries to the higher extremity occur more regularly in youthful children, because of falls, whereas lower extremity injuries happen extra regularly in older children and adolescents (1, 4). Injury surveillance identifies particular risks for particular sports and may result in harm prevention by necessary modifications in tools. Face masks and helmets used in hockey, shin guards utilized in soccer, and helmets used in baseball are examples of apparatus modification put into place after injury surveillance charges indicated the necessity for change. Despite the accidents seen in a sports activities medicine clinic, the documented well being advantages of sports exercise which embody weight management, elevated power, flexibility and endurance, as nicely as improved shallowness outweigh the dangers of great damage. Probably, the most important particular person in guaranteeing damage prevention is the coach. The coach must be qualified in sport-specific strategies of coaching, injury prevention, injury recognition, and correct rehabilitation of the injured athlete before return to participation. An understanding and educated coach could make a long-lasting impression on the athlete, particularly at the youth level. Strength training for particular sports activities is permissible with none concern for overuse damage or effect on development, as lengthy as the program is supervised and submaximal weights are employed. Rehabilitation is a process in which a series of structured actions allow an athlete to return to normal exercise or operate. Although the doctor will make the prognosis and assess the practical limitations of the harm, bodily remedy is actively concerned in the rehabilitation course of to enable the athletes to resume their previous level of activity. The physician ought to supervise the rehabilitation course of and decide when joint functions, muscle strength, and sport-specific features are restored (7). For minimal accidents similar to minor contusions and sprains, the necessity for supervised rehabilitation is questionable. However, for major joint accidents such as vital ligament sprains, fractures, and important resistant overuse syndromes, physical therapy will normally assist the athlete to a speedier return to activity and may also stop additional or repetitive injuries (8). The phases of rehabilitation embrace the preliminary period of acute care when the limb is put at relative relaxation, and pain and irritation are controlled by ice, elevation, and compression (7). The next section, or intermediate phase, is aimed at the resolution of pain and restoration of joint motion, flexibility, and power.
Discount 1000 mg tinidazole visa
A normal lateral strategy is utilized between the triceps posteriorly and the brachialis/extensor carpi radialis longus anteriorly antimicrobial underwear tinidazole 500 mg cheap overnight delivery. Soft-tissue stripping posteriorly ought to be prevented to cut back the risk of avascular necrosis of the capitellum and trochlea antimicrobial over the counter order tinidazole 300 mg otc. Stabilization could be achieved with two clean pins crossing the fracture web site and exiting the alternative cortex. The pins and forged are eliminated three to 6 weeks after surgical procedure, depending on the extent of therapeutic seen on postoperative radiographs. The child was placed in a long-arm cast and a follow-up 1 week later was beneficial. E, F: Radiographs taken in the cast four weeks after open reduction and pinning present anatomic alignment and early therapeutic. Acute swelling and hazard of compartment syndrome are less than in supracondylar humerus fractures. Management of the late-presenting lateral condyle malunion is an space of controversy. Remodeling obscures fracture traces and interferes with restoration of anatomic reduction following osteotomy. Excessive stripping of the condyle to facilitate reduction might lead to avascular necrosis and greater joint stiffness. Two surgical approaches are described within the literature for administration of symptomatic sufferers with malunion. Supracondylar osteotomy, combined with ulnar nerve transposition, has been carried out with passable enchancment in operate (101). Intra-articular osteotomies, with partial reduction, have also achieved passable results (107). Nonunion after lateral condyle fracture is seen most frequently in untreated patients, with displacement of three mm or extra. Delayed union and nonunion has been attributed to fracture instability, publicity to synovial fluid, and decreased vascularity due to the big articular surface of the fracture fragment. Long-term sequelae of nonunion embody ulnar neuritis, progressive valgus deformity, and elbow instability with decreased energy. The amount of bone graft needed is small, and can be obtained from the iliac crest, proximal ulna, or distal radius. Ulnar nerve transposition may be needed, especially if there are preoperative symptoms (108). Asymmetric development of the lateral condyle or incomplete reduction can produce mild cubitus varus. Fishtail deformity, or deepening of the trochlear groove, could outcome from central growth arrest or more likely from avascular necrosis. This deformity rarely compromises short-term function, however could predispose to later condylar fracture (94). Corrective osteoto- mies with nerve decompression or transposition can modify the deformity and symptoms. The medial epicondylar apophysis is fractured when a valgus load is applied to the extended elbow. The displacement is encouraged by the pull of the forearm flexor muscle group, which is hooked up on this region. The medial collateral ligament, which also originates from this apophysis, may play a role within the initial fracture displacement, especially when the fracture is associated with an elbow dislocation. Fracture of the medial epicondyle is essentially dependent on age and is expounded to the ossification of the epicondyle. Ossification begins at roughly 4 to 6 years of age, and fusion occurs at roughly 15 years of age. Early within the course of, the medial epicondyle is part of the entire distal humeral epiphysis. As growth continues, between 9 and 14 years of age this apophysis turns into separated from the principle epiphysis, which is when most of these fractures happen. Almost 50% of medial epicondyle fractures occur concomitantly with posterolateral elbow dislocation. When this occurs, the ulnar nerve can also be within the joint, and vigorous attempts at closed manipulation must be avoided. There is general settlement that surgical intervention is indicated when the epicondyle is trapped within the joint. There are advocates for the closed therapy of this harm whatever the magnitude of displacement (110, 111). Nonunion is a frequent results of closed management, however the nice majority of sufferers are asymptomatic. Valgus instability to stress testing has been suggested as a sign for surgical stabilization (112). However, most contemporary medial epicondyle avulsion accidents will demonstrate instability, so most sufferers will endure surgical procedure if this take a look at is used as an indication. Late instability after closed management has been reported, however this complication is rare until the epicondylar fragment has been excised (111, 112). Excellent outcomes have also been reported after surgical stabilization of reasonably displaced fractures (113). Surgical intervention for lesser degrees of displacement can be considered for competitive athletes in a sport producing elbow valgus stress such as pitching or gymnastics, or in cases of a concomitant elbow dislocation. Many facilities at the moment are difficult this conservative view and are recommending a more aggressive surgical strategy for these fractures. Open Reduction and Internal Fixation of Displaced Lateral Condyle Fracture of the Humerus. The operation is carried out with a tourniquet high on the arm and with the affected person supine. The arm must be positioned on a brief arm board so that picture intensifier views can be obtained to confirm the situation of the pins: the reduction of the fracture, and particularly the articular surface, is visualized directly, so that is one operation by which a headlight is useful. An incision is made instantly over the lateral condyle, about 5 cm in length for young children, and proportionally larger in older children. The landmarks of the lateral condyle could be tough to establish within the youthful baby with a swollen elbow, and one desires to keep away from dissecting too proximally to keep away from the radial nerve. Beneath the pores and skin, a majority of the dissection is often already carried out by the damage. A Chandler retractor or ArmyΎavy retractor throughout to the medial fringe of the joint improves visualization. A key step in visualization is dissection of the distal most soft-tissue attachments from the lateral portion of the capitellum, releasing the anterior capsular attachments to visualize the anterior capitellum. The intact joint surface on each side of the fracture must be seen to obtain an accurate discount. Finally, in preparation for the reduction, the periosteum is trimmed from the distal fragment to allow visualization of the cortical surface so that accurate apposition to the proximal fragment may be achieved. Avoidance of dissection on the posterior facet of the fragment is imperative to avoid interference with its blood supply.
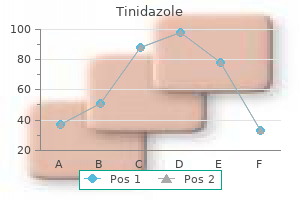
Cheap tinidazole 500 mg visa
The intercalary fragment of femoral shaft created by the 2 osteotomies should now be break up and moved out of the way to allow the femur to shorten antibiotic yeast infection treatment tinidazole 300 mg buy. If the complete piece of bone or one giant piece of bone is displaced infection 0 mycoplasme order tinidazole 300 mg without prescription, it could create a symptomatic enlargement that interferes with muscle movement. The intramedullary chisel is inserted by way of the proximal and intercalary fragments, and the hook is directed posterolaterally to catch on a thick a part of the intercalary fragment. It is normally not potential to break up the linea aspera, and if the thin anterior cortex is split, one massive and one small fragment will result. With the hook within the correct location, the slotted hammer is used to drive the hook out of the canal. The image intensifier is used to verify that the intercalary fragment is break up and to keep away from splitting the proximal femoral shaft. After the fragment is split, the hook is used to displace the items to all sides. It should be attainable to displace the cut up fragments and convey the distal and proximal shaft into apposition. Less than inflexible fixation can result in lack of rotational management and opening of the shortening hole, two problems that are troublesome to control with out locking. It leaves a small, cosmetically acceptable scar, and the later process to take away the rod is of lesser magnitude than that required to remove a blade plate. E: the cylinder of bone has been break up with the osteotomes, F: Femoral nail fixation is carried out after the femur is shortened. Patients with higher shortening require 6 to 12 months to regain regular knee management and performance (169). This methodology is appropriate for sufferers with concomitant proximal femoral deformity that wants to be simultaneously corrected. This methodology could additionally be greatest for sufferers who may not be nice candidates for intramedullary fixation. This has the benefit of minimizing the degree of quadriceps useful lengthening and subsequently minimizing postoperative weak spot. Mid diaphyseal shorten- ings have the disadvantage of weakness in addition to probably decreased healing seen in nonmetaphyseal bone. Today, a bunch of different fixation choices can be utilized and embrace units with proximal fixation into the femoral neck (pediatric sized hip-screw gadgets or blade plates). We prefer to use a 110- or 130-degree plates so as to stabilize the femur; these devices have a decrease profile than hipscrew gadgets or 90-degree blade plates which are more appropriate for varus osteotomy (varus plates are designed for medial displacement of the femoral shaft). With these implants, we can perform an osteotomy on the junction of the intertrochantericγubtrochanteric degree. This method combines some great benefits of metaphyseal healing with out significantly affecting the Blix curve of the quadriceps function. A lateral approach to the proximal femur is made, the fascia lata is incised, and the vastus lateralis is indifferent from the vastus ridge and elevated posteriorly to preserve an anteriorly based flap of muscle. She is a poor candidate for external fixation as a end result of dangers of infection and her severe immunodeficiency. B: Distal osteotomy is required to right deformity, but proximal femoral shortening osteotomy is moreover chosen as a end result of concerns for weak spot from shortening distally. D: Good knee extension is feasible secondary to preservation of her in situ quadriceps length. Failing to advance the chisel on this cyclical means can lead to great problem in eradicating the chisel as quickly as the bone has been sectioned. After the chisel website has been appropriately prepared and the chisel seated, the osteotomy stage is planned; the most proximal cut is positioned at or above the level of the lesser trochanter. The distal level is measured and equally cut and the middleman bone segment is eliminated. The chisel is eliminated and the blade plate is positioned proximally along the chisel path; the plate is then fastened to the distal shaft after concurrently shortening the bone while sustaining in situ rotation. The bone that was eliminated could be ground up and used as bone graft at the osteotomy degree prior to wound closure. Partial development arrests (bar or bridge) are a consequence of localized growth plate injury ensuing from a giant number of etiologies including trauma, an infection, or neoplasm. Growth arrests can range in measurement and location and lead to variable combinations of angular deformity or limb-length discrepancy. For occasion and compared to traumatic development arrests, the bridge from infections tends to be much less discrete, bigger and more central, and might even consist of multiple small bridges. The latter is extraordinarily sensitive and in instances the place no obvious deformity (length discrepancy or angulation) has resulted, the surgeon could be clever to document irrefutable growth alteration earlier than considering therapy. Bridge resections are often limited to those that contain <50% of the floor space of the growth plate and who would have at least a 2-cm discrepancy at maturity. In sufferers who would have less than a 2-cm discrepancy at maturity, completion of the growth arrest is preferable to the unpredictable results inherent to bridge excision. Attempted excision of bars >50% could also be thought of in selected circumstances the place the anticipated growth loss is >5 cm. In these younger sufferers, an try at excision may be preferred to the tough therapy of limb lengthening. Established bars could be thought of peripheral or central, the latter are tougher to remove and treat. In order to take away a central bar, a gap is made in the metaphysis and the bone is eliminated distally until the physeal scar is approached. Circumferential removing of bony bar at the degree of the expansion plate will proceed until growth plate is visualized for 360 degrees; this can be facilitated with the utilization of an arthroscope digital camera (170) or a dental mirror. The resected space is then full of inert materials corresponding to fat or cranioplast cement (minimally exothermic bone cement). Peripheral bars are exposed and the margins of the bar are outlined with intraoperative imaging and from preoperative planning. Under loupe magnification and headlight illumination, the bone is burred away until progress plate is current at all areas. Once the bone is removed, inert material (fat or cranioplast) is placed into the defect and can forestall the bone from rising again between the epiphysis and the metaphysis. Placement of k-wires within the epiphysis and the metaphysis will facilitate monitoring of the growth plate operate. Patients with discrepancies >6 cm may solely require limb lengthening as a component of their discrepancy. Patients with discrepancies higher than this may require a quantity of and different operations (including limb lengthening) and are higher termed limb reconstruction candidates. Correction of projected discrepancies of 15 to 20 cm is feasible with latest advances in technology and with improved understanding of mechanisms or methods to avoid or cut back the morbidity related to these endeavors (171ͱ73). In order to correct deficiencies of this magnitude, the patient and their families need to remember that a series of operations could also be wanted to optimize the limb (limb optimization) prior to limb lengthening and that increases in length are finest obtained with a sequence of reasonable lengthening attempts (10% to 20% in size at each limb-lengthening attempt). Thus, an exterior fixator interval of as much as 6 months might be required and can precede many extra months of required rehabilitation.
Diseases
- Pai Levkoff syndrome
- Acute myeloblastic leukemia type 4
- Polyarthritis, systemic
- Leukocyte adhesion deficiency type 2
- Glossopharyngeal neuralgia
- Pseudoachondroplastic dysplasia 1
- Shprintzen Golberg craniosynostosis
- Aneurysm of sinus of Valsalva
- Swyer James and McLeod Syndrome
1000 mg tinidazole order
All of Langenskis sufferers have been Caucasians from Finland virus 68 map tinidazole 1000 mg proven, whereas a large proportion of sufferers in the United States are African American antibiotics for sinus and lung infection tinidazole 1000 mg order with amex. North American kids sometimes expertise extra rapid progression with more extreme, irreversible adjustments at an earlier age than their European counterparts. The higher incidence and severity of illness has been attributed to a higher proportion of overweight children in North America (80). It may be a response to the asymmetric load throughout the knee, allowing relative overgrowth of the distal medial femur (52, 66). More typically, the valgus look of the femur is a consequence of extreme tibial bowing and relative abduction of the hip, which creates the illusion of valgus on the distal femur. In contrast, brace treatment was less profitable for treating bilateral deformities, with solely 18 of 28 patients famous to be successfully treated. Compliance was far more difficult to achieve for the child with bilateral deformity, as is comprehensible. Thigh and calf cuffs and a varus-correcting lateral knee pad present three-point fixation. Brace remedy is continued until the bony adjustments in the proximal medial tibia resolve; typically, this takes 1� to 2 years of brace remedy (75ͷ7). Brace therapy shall be profitable if by 4 years of age the mechanical axis of the decrease extremity passes via the center of the knee and the despair of the medial epiphysis resolves. The radiographic appearance of the medial epiphysis and metaphysis ought to normalize by 5 years of age. Alternatively, surgical remedy with development modulation has been shown to be effective in chosen instances. Surgical therapy unloads the medial compartment of the knee and facilitates the expansion of the proximal medial physis. Restoration of regular progress in the medial tibial physis is less likely to occur if surgery is delayed corresponding to till 5 years of age (78). Growth modulation is greatest accomplished on this age affected person with the placement of a smallfragment (typically two-hole) plate extraperiosteally throughout the proximal lateral tibial physis. This is assessed by measuring the mechanical axis of the concerned lower extremity. With correction of the varus deformity, the mechanical axis will shift from its earlier location medial to the middle of the knee to a more lateral position. Additional risk factors include obesity, ligamentous instability, or the presence of a lateral thrust, any of which can potentiate a varus deformity (51, 54). Studies have demonstrated that brace therapy can correct both the varus deformity and the pathologic proximalέedial tibial progress disturbance (75ͷ7). Slight overcorrection is fascinating to compensate for the customarily occurring and variable differential progress of the proximal tibial physis. Continued follow-up is mandatory to assure that correction of varus is maintained and/or to handle recurrent deformity. Repeat software of the plate may be needed to appropriate delicate recurrent deformity. The proximal tibial osteotomy is carried out with consideration to each the identified inherent risks and the necessity for acquiring sufficient correction of the deformity (78, eighty, 81). The fibula is osteotomized by way of a separate lateral incision, taking care to avoid injury to the deep motor branches of the peroneal nerve (38, 82). The tibial osteotomy could be completed in a selection of strategies (48, fifty one, sixty eight, seventy eight, 826). A straight transverse osteotomy allows for essential correction of frontal, sagittal, and rotational deformity. A slight "overcorrection" into valgus with or without translation of the distal fragment laterally is fascinating (48, 50, 51, 82). This locations the mechanical axis of the leg within the lateral compartment of the knee, unloading the medial proximal tibia. The mechanical axis of the leg may be assessed intraoperatively using the bovie wire. The cord is stretched from the center of the hip and across the middle of the ankle with the leg resting on a radiolucent desk. This easy technique supplies a reproducible method to confirm that the mechanical axis has truly been transferred lateral to the middle of the knee joint (82). If a unilateral deformity is current, medical comparison to the conventional extremity is helpful in figuring out whether or not enough correction has been obtained. A subcutaneous fasciotomy of the anterior compartment is carried out previous to wound closure. Postoperatively, the extremity is immobilized in a non weight-bearing, long-leg, bent-knee forged. Alternatively, a spica solid is used for the child with relatively brief, fat extremities. Following corrective osteotomy, the pathologic adjustments within the proximal medial tibia must be rigorously monitored. Prophylactic restricted fasciotomy and using drains assist avoid increased compartment strain (38, eighty two, 89). If a compartment syndrome is suspected postoperatively, instant fasciotomy ought to be performed. Based on our previous medical expertise, an acute traction or impingement damage to the peroneal nerve can also happen (38). Prompt surgical release of any peroneal nerve compression has typically resulted in a satisfactory end result. Recurrent or worsening varus deformity with persistent pathologic modifications can happen regardless of restorative osteotomy at a younger age (44, 50, 51). Identification of a bar may be difficult because of the serpentine course of this abnormal physis, which takes on a vertical slope as the deformity worsens. This occurs somewhat subtly due to a decreased development price of the proximal medial tibial physis relative to the lateral physis and can happen any time previous to skeletal maturity. As the physis transitions from a standard horizontal orientation to a extra vertical place, this differential progress turns into more evident. Careful observation is required to detect this modification early in the midst of treatment. Premature closure of the medial tibial physis regularly occurs because of persistent deficient proximal medial physeal development. If this occurs, the varus deformity can usually be controlled with progress modulation, utilizing an eight-plate or hemiepiphyseal staples (48, seventy nine, 90, 91). If further tibial physeal growth is anticipated, the interior fixation is eliminated after a slight overcorrection is obtained. Careful follow-up together with radiographic evaluation of recurrent varus deformity and/or leg-length inequality are obligatory till skeletal maturity is reached.
Cheap tinidazole 300 mg on-line
Some practitioners favor operative treatment in teenage athletes to facilitate rehabilitation and perhaps earlier return to sport virus 68 california tinidazole 1000 mg buy overnight delivery, particularly in circumstances the place the clavicle fracture is on the dominant aspect of a throwing athlete antibiotics gel for acne cheap tinidazole 1000 mg line. Two latest papers have famous that kids and adolescents could be treated efficiently with plate fixation with very low complication rates (3, 4). In adolescent sufferers, a "wait-and-see" method identified four sufferers with displaced clavicle fractures who developed symptomatic malunions. Nonunion after clavicle fracture has been reported in adolescents, however it responds to bone grafting and plating (5). Posterior or retrosternal displacement of the medial clavicle could cause harm to or compress the nice vessels, trachea, or esophagus, and thus reduction is indicated. The swelling and dorsal prominence of the clavicle could counsel an acromioclavicular separation. However, the distal epiphysis of the clavicle and the acromioclavicular joint remain reduced. An anterior strategy is beneficial for anterior glenoid fractures, and a posterior method is used for scapular neck and glenoid fossa fractures (21). Less than 2% of glenohumeral dislocations happen in patients youthful than 10 years (22). Atraumatic shoulder dislocations and chronic shoulder instability are discussed elsewhere on this e-book. Approximately 20% of all shoulder dislocations occur in persons between the ages of 10 and 20 years. Most displace anteriorly and produce a detachment of the anteroinferior capsule from the glenoid neck. Treatment of traumatic shoulder dislocation in children and adolescents is nonsurgical, with light closed reduction. This is completed by offering sufficient ache aid, muscle relaxation, and gravity-assisted arm traction in the susceptible place. An alternative methodology is the modified Hippocratic technique in which traction is utilized to the arm while countertraction is applied utilizing a folded sheet across the torso. After discount, a shoulder immobilizer or sling is used for 2 to three weeks earlier than initiating shoulder muscle strengthening. The most frequent complication is recurrent dislocation, which has an incidence between 60% and 85%, normally within 2 years of the first dislocation (23, 24). Posterior dislocations of the shoulder may recur and require surgical stabilization in youngsters (25). A more detailed discussion of this damage and its treatment is found elsewhere in this guide. The proximal humeral physis stays open in ladies until 14 to 17 years of age and in boys until sixteen to 18 years of age. Mechanisms of damage that might produce a shoulder dislocation in adults normally end in a proximal humeral fracture in youngsters and adolescents. Metaphyseal fractures are extra common earlier than the age of 10, and epiphyseal separations are extra widespread in adolescents. The distal fragment often displaces within the anterior direction as a end result of the periosteum is thinner and weaker in this area. The proximal fragment is flexed and externally rotated because of the pull of the rotator cuff, whereas the distal fragment is displaced proximally because of the pull of the deltoid muscle. Remarkably, it is a comparatively benign damage due to the speedy fee of remodeling with progress and the wide range of shoulder movement (26, 27). The lengthy head of the biceps may be interposed between the fracture fragments and may impede discount (28). They are managed in a shoulder immobilizer for 3 to 4 weeks, followed by range-of-motion workouts and gradually elevated activity. These fractures are tough to cut back and keep in a decreased place by closed methods. Current choices for administration embrace immobilization with out making an attempt discount, or discount under sedation or anesthesia with evaluation of postreduction stability, and percutaneous fixation if unstable. Some practitioners additionally believe that accidents to the dominant arm of a throwing athlete must also be treated with discount and fixation. If unstable, the fracture was treated with percutaneous pin fixation and immobilization. The indications for operative management of adolescent proximal Closed Reduction Method. In most fractures, the distal fragment shall be displaced anteriorly through the thinner periosteum, and the proximal fragment will be kidnapped and externally rotated by its muscular attachments. After sufficient analgesia and/or anesthesia, longitudinal traction is utilized to the injured extremity, and the distal humeral fragment is flexed, abducted, and externally rotated. Posteriorly directed stress during flexion on the distal fragment will push it again contained in the soft-tissue envelope, after which abduction and external rotation will cut back the fragment. Fluoroscopy is useful to assess the place of the fracture fragments during discount. If the fracture redisplaces to an unacceptable diploma with the arm at the facet, then repeat reduction and percutaneous pin fixation is warranted. For minor quantities of residual varus, an abduction pillow at the facet with the sling and swathe may be used. For unstable fractures and irreducible fractures, the affected person must be taken to the working room for basic anesthesia. The patient is positioned supine at the edge of a very radiolucent table to facilitate fluoroscopy. The arm and shoulder are sterilely prepared and draped, and repeat closed discount is tried. Because of the risk of migration with use of easy pins, some prefer pins with threaded tips, and it is recommended to place a big bend ultimately of the pins left outside the skin. The axillary nerve is in danger, and runs from posterior to anterior across the proximal humerus in a zone 5 to 7 cm distal to the tip of the acromion. Pins should thus begin distal to this, and are placed from the lateral proximal humeral metaphysis and directed up and into the humeral epiphysis. The first pin begins anterolaterally, and then a second pin is positioned anterior or posterior to the primary, with an attempt to get some divergence or spread of the pins in the epiphysis to enhance stability. HΊ: the patient has recovered full range of motion, but has a 1-cm arm-length discrepancy. The proximal fragment is abducted and externally rotated because of the rotator cuff attachments. The shaft is displaced proximally by the pull of the deltoid muscle and is generally adducted by the action of the pectoralis muscle.
Discount 1000 mg tinidazole
The two rotational deformities are in opposite directions and cancel one another out antibiotic resistance food safety tinidazole 300 mg purchase free shipping. It is essential to talk about this with the affected person and family antibiotic half life order 1000 mg tinidazole fast delivery, because the exterior tibial torsion will become obvious after correction of the foot deformity. Despite variations within the patterns of muscle imbalance that create cavovarus, the sample of deformity development is fairly constant (47ʹ9). The first metatarsal becomes plantar-flexed, giving the appearance of pronation of the forefoot on the hindfoot. The hindfoot must assume a varus position when weight bearing if the primary metatarsal is fastened in plantar flexion (9). Fifth metatarsal makes contact via supination of the forefoot (arrow), which also drives the hindfoot into varus. Flexible deformities are handled with tendon transfers, and inflexible deformities are handled with soft-tissue releases, osteotomies, and, sometimes, arthrodeses. The affected person stands with a block of wood under the lateral border of the foot to recreate the tripod whereas allowing the first metatarsal to plantar-flex. In the primary situation, surgical procedure for deformity correction is confined to the forefoot. The calcaneus is dorsiflexed and vertically aligned, giving it the appearance of posterior truncation. The plantar heel pad is thickly callused from excessive pressure over a small surface space. The incompletely ossified bones change shape because of extreme compression on their plantar aspects (Hueter-Volkmann law). Bearing weight on the plantar-flexed first metatarsal causes the forefoot to supinate in relation to the tibia, thereby permitting the fifth metatarsal head to touch the ground. This flexible hindfoot varus deformity finally becomes rigid because the plantar-medial gentle tissues of the subtalar joint contract. The cavovarus foot, due to this fact, has two major rotational deformities in reverse directions from each other: pronation of the forefoot and supination (varus and inversion are different descriptive terms) of the hindfoot. The flexible varus deformity of the hindfoot (A) corrects to valgus (B) when the plantar-flexed first metatarsal is allowed to drop down off the edge of the block of wooden as in this example. Failure to appropriate to valgus indicates the need for surgical correction of the hindfoot deformity, in addition to the procedures on the forefoot. A: Transtarsal cavus with thick callosities underneath the calcaneus and the metatarsal heads. Lateral radiograph of a cavovarus foot deformity earlier than (A) and after (B) a medial cuneiform plantar-based opening-wedge osteotomy. The flexibility or rigidity of the subtalar joint can be documented by assessing alignment at the talonavicular joint using the talusΦirst metatarsal angle. B: With block, the hindfoot varus is corrected as indicated by abduction of the 1st metatarsal axis in relation to the axis of the talus. The weakened lumbricals allow the lengthy toe extensors to prolong the metatarsophalangeal joints and the lengthy toe flexors to flex the interphalangeal joints, thereby creating claw toe deformities. The intrinsic muscular tissues endure atrophy, fibrosis, and shortening that lead to secondary contracture of the plantar fascia. This creates a bowstring between the anterior and posterior pillars of the arch that draws them nearer and produces equinus of the forefoot on the hindfoot. The tibialis anterior, a dorsiflexor of the first metatarsal, becomes weak, whereas the peroneus longus, a plantar flexor of the primary metatarsal, remains relatively strong (42). The extensor hallucis longus is involuntarily recruited in an attempt to provide additional dorsiflexion power alongside the medial column of the foot, nevertheless it creates a paradoxical impact of plantar flexion because of the windlass effect of the plantar fascia. The tripod effect (48) accounts for the varus position that the hindfoot should assume throughout weight bearing as a result of the fastened pronation of the forefoot. Also contributing to the varus deformity of the hindfoot is the muscle imbalance between the tibialis posterior, an invertor of the subtalar joint, that remains sturdy and the peroneus brevis, an evertor of the subtalar joint, that turns into weak (47). The subtalar joint eventually becomes rigidly deformed in varus due to contracture of the plantar-medial soft tissues, including these of the subtalar joint complicated. Contracture of the plantar fascia, elongation of the paralyzed triceps surae, and preservation of practical energy within the tibialis anterior contribute to the dorsiflexion posture of the calcaneus. Muscle imbalance from each static and progressive neuromuscular issues results in progressive increase within the severity and stiffness of cavus foot deformities, though the rate of progression varies significantly. Treatment of the underlying neurologic dysfunction should precede remedy of the foot deformity. In most instances, cavus deformity is the outcomes of the issue (a neurologic disorder), not the first problem itself. There is little position for nonoperative management of the cavus deformity because most are progressive and of a sophisticated degree of severity at the time of analysis. The complexity of reconstruction increases with the severity and rigidity of the deformities (48, fifty four, 55). Inexpensive, accommodative arch helps and shoe modifications could additionally be used to ameliorate symptoms through the time it takes to diagnose and, if attainable, to treat the underlying etiology. Operative indications embrace evidence of a progressive deformity, painful callosities underneath the metatarsal heads or base of the fifth metatarsal, and hindfoot/ankle instability. The primary principles of surgical administration of a cavus foot are to (a) right all the segmental deformities and (b) stability the muscle forces. Correcting the deformities without balancing the muscle forces (through tendon transfers) will lead to recurrence of the deformities. Conversely, balancing the muscle forces (through tendon transfers) with out correcting the structural deformities will create well-balanced deformities. Correction of deformities lends itself more readily to an algorithm than does muscle balancing. And balancing muscle tissue in a mobile foot is tougher than in one which has undergone subtalar or triple arthrodesis. The third precept of surgical management is to depart affordable therapy choices available for the attainable recurrence of deformity and ache. Because the foot deformity is the result of the (neurologic) drawback and never the primary problem, recurrence of deformity is likely. There is a very lengthy list of operative procedures that might be employed to appropriate the individual deformities and balance the muscle forces within the cavus foot (42, 48, 56ͷ4). The cavus foot deformity should be categorised based mostly on the flexibleness of the segmental deformities. Correction of deformities begins with soft-tissue releases, corresponding to fasciotomies, capsulotomies, and muscle or tendon lengthenings, with the aim of realigning joints (48, fifty five, 58, 60). An osteotomy of the medial cuneiform can be completed through a distal extension of the incision. Osteotomies are employed to appropriate these bone deformities that can solely be recognized following soft-tissue releases and realignment of the joints. The first ray becomes plantar-flexed early in the middle of growth of the cavovarus foot deformity. A airplane is developed between the plantar fascia and the subcutaneous fats of the heel pad at the transverse degree of the lateral plantar neurovascular bundle.
1000 mg tinidazole discount otc
In recent stories by Stevens (143) chest infection tinidazole 300 mg buy free shipping, none of his sufferers had premature growth arrest or rebound when treated with momentary physeal stapling for genu valgum antibiotics for uti without penicillin cheap 1000 mg tinidazole visa. Complications related to osteotomy include failures of union or fixation, an infection, blood loss, knee stiffness, and scar formation. None of those is exclusive to distal femoral or proximal tibial osteotomy for valgus correction. Mobility of the peroneal nerve is limited above the knee because it passes across the distal femur and throughout the lateral fringe of the biceps femoris tendon and below the knee as it curves across the proximal fibula and thru the crural fascia (38). More severe deformities could require launch of one or more of those sites to scale back the risk of permanent damage. Closing-wedge approach for quick correction is much less more likely to stretch the peroneal nerve than opening wedge. Gradual correction of extreme deformities as can be achieved with a round external fixator may permit the nerve to accommodate to these changes more safely than does acute correction. A lateral incision is made alongside the midline of the distal femur from the joint line, extending proximally to accommodate the size of plate to be used. In skeletally immature patients, the osteotomy and fixation are proximal to the physis and a contoured plate is used. The method described here is for skeletally mature sufferers and uses a blade plate for fixation. The iliotibial band is incised according to the midline of the femur and the vastus lateralis is identified distally and elevated from the fascia utilizing a periosteal elevator. The exposure of the femur can be prolonged by adding transverse cuts in the periosteum, proximally and distally. A clean Kirschner wire is placed across the femoral condyles to information placement of the chisel within the distal femur. The drill jig can be used to place 3 drill holes used to set up a small trough within the lateral cortex where the chisel shall be inserted. The seating chisel is inserted taking care to adjust the angle and rotation to allow correct contact of the blade plate with the shaft of the femur. For correction of a valgus deformity, reduction of the plate along the shaft of the femur, creating a gap wedge, corrects the deformity. Alternatively, a wedge is eliminated for correction of a varus based mostly on a template of the pre-operative radiograph. The washers may be tied together using absorbable suture and positioned between the plate and bone while screws are inserted. The patient is toe-touch weightbearing for six weeks, with weight-bearing superior based on healing of the osteotomy. In skeletally immature sufferers, the osteotomy and fixation are completed proximal to the physis. The dimension of a gap or closing wedge osteotomy is decided using a template of the preoperative radiograph. Bowing of the tibia that presents at start usually is both anterior, anterolateral, or posterior medial. Anterior tibial bowing that occurs in affiliation with a poor or absent fibula is diagnostic of fibular hemimelia. Posterior medial bowing occurs in association with calcaneovalgus foot deformity and has a great prognosis. In distinction, anterolateral bowing, which usually presents quickly after delivery, is often a progressive deformity which regularly leads to a pseudarthrosis. Neurofibromatosis occurs in more than 50% of sufferers with anterolateral bowing, with or without pseudarthrosis of the tibia (144ͱ48). This bowing will be the first medical manifestation of neurofibromatosis (146, 147). Both noted the variable natural historical past and prognosis of each of the kinds they described (Table 27. Once the analysis of anterolateral bowing is made, full-time brace treatment is indicated. Surgical therapy of an intact pathologic anterolaterally bowed tibia within the toddler and/or younger baby should be avoided. Once an apparent pseudarthrosis is established, surgical remedy can be thought-about. A current series of 10 sufferers with neurofibromatosis and pre-pseudarthrosis had been successfully managed with fibular allograft and long-term orthotic use (152). These distinctive patients seem to carry less likelihood of progression and fracture following the bone graft procedure. Rather, the tibia with an anterolateral bow appears dysplastic, with failure of tubulation, cystic prefracture, or frank pseudarthrosis, or a mix of those features, with narrowing of the fragments (144, 146). Once established, the pure history of a pseudarthrosis is that of persistent instability and progressive deformity. Numerous classification systems have been proposed in an try to predict the natural historical past and outcome of remedy. A: Anterolateral bowing of the tibia could additionally be obvious at start or could progress with weight bearing. The adjoining bone could appear sclerotic, with increased density, or it might be atrophic and spindle formed. Once the deformity is acknowledged, the leg should be protected with a total contact orthosis. B: Fracture happens on the apex of the bow, often with out prodromal signs and with minimal or no trauma. Even with consolidation, the tenuous standing of the atrophic bone markedly limits practical potential (144ͱ46). Less invasive technical innovations had been developed by Brighton and Bassett (157, 158) utilizing implanted cathode leads or pulsed electromagnetic present, either alone or in combination with surgical stabilization. However, even after obtaining consolidation with any of those strategies, long-term follow-up is crucial to tackle related deformities that frequently happen later in the course of the illness. These embrace refracture, persistent or increasing valgus deformity, and limb-length inequality. A posterior iliac bone graft is obtained consisting of adequate corticocancellous strips and cancellous bone graft. The pseudarthrosis is excised and the bone fragments stabilized with a Williams rod (162, 165). The desired foot place is neutral dorsiflexion/plantarflexion verified clinically and with the C-arm. The tibial fragments are anatomically decreased on the pseudarthrosis website, and the rod is driven retrograde into the proximal fragment. In smaller kids and people with distal defects, fixation throughout the ankle joint for 1 to 2 years may be fascinating to reduce stress on the pseudarthrosis web site, which facilitates consolidation. Proximally, the rod ought to stay inside the proximal tibial metaphysis and never cross the physis. The rod may be advanced across the ankle joint as soon as the defect has united (typically not until 2 years following placement) to allow ankle motion. A: After excision of the pseudarthrosis, the Williams rod is inserted, antegrade, through the distal tibia, talus, and calcaneus and exits through the heel pad.