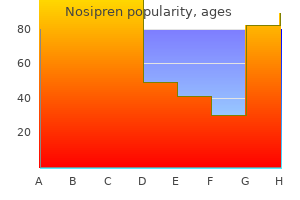
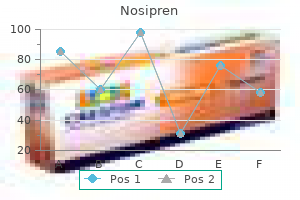
Nosipren dosages: 40 mg, 20 mg, 10 mg, 5 mg
Nosipren packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills
Buy nosipren 40 mg otc
In common allergy shots dc discount nosipren 20 mg with visa, extrinsic muscle tissue alter the place of the tongue allergy symptoms late summer nosipren 40 mg on-line, and intrinsic muscles alter its form. The four intrinsic and 4 extrinsic muscles in each half of the tongue are separated by a median fibrous lingual septum. The extrinsic muscular tissues of the tongue (genioglossus, hyoglossus, styloglossus, and palatoglossus) originate exterior the tongue and attach to it. The superior and inferior longitudinal, transverse, and vertical muscular tissues are confined to the tongue. The superior and inferior longitudinal muscle tissue act together to make the tongue brief and thick and to retract the protruded tongue. The transverse and vertical muscles act simultaneously to make the tongue lengthy and slim, which may push the tongue against the incisor tooth or protrude the tongue from the open mouth (especially when appearing with the posterior inferior a part of the genioglossus). The chorda 2127 tympani joins the lingual nerve within the infratemporal fossa and runs anteriorly in its sheath. These principally sensory nerves also carry parasympathetic secretomotor fibers to serous glands within the tongue. Traditionally, four fundamental taste sensations are described: sweet, salty, bitter, and bitter. A fifth primary taste (umami-stimulated by monosodium glutamate) has more just lately been recognized. Certain areas of the tongue have been described as being most delicate to the completely different tastes, but evidence indicates all areas are able to detecting all tastes. Other "tastes" expressed by gourmets are influenced by olfactory sensation (smell and aroma). The dorsal lingual arteries supply the root of the tongue; the deep lingual arteries provide the body of the tongue. The deep lingual arteries communicate with each other close to the apex of the tongue. The dorsal lingual arteries are prevented from speaking by the lingual septum. The main artery to the tongue is the lingual artery, a department of the external carotid artery. The dorsal lingual arteries provide the blood supply to the basis of the tongue and a department to the palatine tonsil. The sublingual 2129 arteries provide the blood provide to the floor of the mouth, including the sublingual glands. The veins of the tongue are the dorsal lingual veins, which accompany the lingual artery. The deep lingual veins, which start at the apex of the tongue, run posteriorly beside the lingual frenulum to be a part of the sublingual vein. The sublingual veins in aged persons are often varicose (enlarged and tortuous). Most of the lymphatic drainage converges toward and follows the venous drainage; however, lymph from the tip of the tongue, frenulum, and central decrease lip runs an unbiased course. Lymph drains to the submental, submandibular, and superior and inferior deep cervical lymph nodes, including the jugulodigastric and jugulo-omohyoid nodes. Lymph from the basis of the tongue drains bilaterally into the superior deep cervical lymph nodes. Lymph from the medial a half of the body drains bilaterally and on to the inferior deep cervical lymph nodes. Lymph from the right and left lateral elements of body drains to the submandibular lymph nodes on the ipsilateral side. The apex and frenulum drain to the submental lymph nodes, the medial 2132 portion draining bilaterally. All lymph from the tongue in the end drains to the deep cervical nodes and passes by way of the jugular venous trunks into the venous system on the proper and left venous angles. Salivary Glands the salivary glands are the parotid, submandibular, and sublingual glands. The clear, tasteless, odorless viscid fluid, saliva, secreted by these glands and the mucous glands of the oral cavity retains the mucous membrane of the mouth moist. The parotid glands, the largest of the three paired salivary glands, were discussed earlier on this chapter. The parotid glands are situated lateral and posterior to the rami of the mandible and masseter muscular tissues, inside unyielding fibrous sheaths. The submandibular duct, roughly 5 cm lengthy, arises from the portion of the gland that lies between the mylohyoid and hyoglossus muscle tissue. Passing from lateral to medial, the lingual nerve loops under the duct that runs anteriorly, opening by one to three orifices on a small sublingual papilla beside the base of the frenulum of the tongue. The orifices of the submandibular ducts are visible, and saliva can often be seen trickling from them (or spraying from them throughout yawning). The arterial provide of the submandibular glands is from the 2133 submental arteries. The lymphatic vessels of the glands end within the deep cervical lymph nodes, particularly the jugulo-omohyoid node. Fine ducts passing from the superior border of the sublingual gland open on the sublingual fold. The proper sublingual and submandibular glands and the ground of the mouth are shown. The orifice of the duct of the submandibular gland is seen on the anterior end of the sublingual fold. The sublingual carunculae are bilateral papillae flanking the frenulum of the tongue, every bearing the opening of the ipsilateral submandibular duct. The submandibular glands are provided by presynaptic parasympathetic secretomotor fibers conveyed from the facial nerve to the lingual nerve by the chorda tympani nerve, which synapse with postsynaptic neurons in the submandibular ganglion. The latter fibers accompany arteries to reach the gland, along with vasoconstrictive postsynaptic sympathetic fibers from the superior cervical ganglion. Each almond-shaped gland lies in the floor of the mouth between the mandible and the genioglossus muscle. The glands from both sides unite to kind a horseshoe-shaped mass around the connective tissue core of the frenulum of the tongue. Numerous small sublingual ducts open into the floor of the mouth along the sublingual folds. The arterial supply of the sublingual glands is from the sublingual and submental arteries, branches of the lingual and facial arteries, respectively. Presynaptic parasympathetic secretomotor fibers are conveyed by the facial, chorda tympani, and lingual nerves to synapse within the submandibular ganglion.
Discount nosipren 10 mg otc
Although these vestigial structures are mostly of embryological and morphological interest allergy medicine kroger nosipren 5 mg buy generic on-line, they often accumulate fluid and form cysts allergy austin nosipren 40 mg purchase without prescription. Bicornate Uterus Incomplete fusion of the embryonic paramesonephric ducts, from which the uterus is fashioned, ends in a wide range of congenital anomalies, starting from formation of a unicornuate uterus (receiving a uterine duct solely from the proper or left) to duplication in the type of a bicornate uterus. Disposition of Uterus Normally, the uterus is anteverted and anteflexed, so that the body of the uterus rests upon the empty bladder, considered one of a quantity of means by which passive support for the uterus could also be provided. However, the uterus could assume other inclinations, together with excessive anteflexion. Once marked, retroversion and/or retroversion was thought to be a potential predisposing consider uterine prolapse or to current a potential complication in being pregnant; nevertheless, this has proven to be unjustified. Manual Examination of Uterus the dimensions and disposition of the uterus could also be examined by bimanual palpation. When softening of the uterine isthmus happens (Hegar sign), the cervix feels as if it were separated from the body of the 1436 uterus. Lifetime Changes in Anatomy of Uterus 1437 the uterus is probably essentially the most dynamic structure in human anatomy. At start, the uterus is relatively large and has grownup proportions (body to cervical ratio = 2:1) as a outcome of the prepartum (before childbirth) affect of the maternal hormones. Several weeks postpartum (after childbirth), childhood dimensions and proportions are obtained: the body and cervix are approximately of equal length (body to cervical ratio = 1:1), with the cervix being of greater diameter (thickness). Because of the small size of the pelvic cavity throughout infancy, the uterus is especially an stomach organ. The cervix remains relatively giant (approximately 50% of whole uterus) throughout childhood. During puberty, the uterus (especially its body) grows rapidly in measurement, once once more assuming adult proportions. In the postpubertal, premenopausal, nonpregnant girl, the body of the uterus is pear shaped; the thick-walled superior two thirds of the uterus lies within the pelvic cavity. During this phase of life, the uterus undergoes monthly changes in size, weight, and density in relation to the menstrual cycle. Over the 9 months of being pregnant, the gravid uterus expands significantly to accommodate the fetus, becoming bigger and more and more skinny walled. The uterus becomes almost membranous, with the fundus dropping beneath its highest degree (achieved in the 9th month), at which period it extends superiorly to the costal margin, occupying a lot of the abdominopelvic cavity. Immediately after delivery of the fetus, the big uterus turns into thick walled and edematous. The multiparous nongravid uterus has a big and nodular body and often extends into the lower stomach cavity, often inflicting a slight protrusion of the inferior stomach wall in lean ladies. During menopause (45�55 years of age), the uterus (again, particularly the body) decreases in size. All these levels represent normal anatomy for the actual age and reproductive standing of the woman. Cervical Cancer Screening Until 1940, cervical most cancers was the main explanation for demise in North American women (Krebs, 2000). The decline within the incidence and number of girls dying from cervical cancer is said to the accessibility of the cervix to direct visualization and to cell and tissue study via cervical cytology (invented in 1946 by Dr. Cervical cytology permits detection and therapy of premalignant cervical situations (Hoffman et al. The vagina can be distended with a vaginal speculum to enable inspection of the cervix. The spatula is rotated to scrape cellular materials from the mucosa of the vaginal cervix. The mobile materials is then placed in a preservative liquid for microscopic examination. Because no peritoneum intervenes between the anterior cervix and the bottom of the bladder, cervical cancer could unfold by contiguity to the bladder. The incidence of hysterectomy for noncancerous causes has markedly declined in favor of exploring different options. The procedure stops abnormal bleeding but in addition stops menstrual periods and ends the ability to conceive. The incidence of 1440 hysterectomy for noncancerous reasons has markedly declined in favor of exploring different options. Depending on the location, extent, and nature of the pathology, a subtotal (supracervical or cervical), complete, or radical hysterectomy could additionally be carried out, the latter involving elimination of the ovaries along with the uterus. When cervical or total hysterectomies are carried out, the vaginal fornices are incised, encircling the cervix, to separate the uterus from the vagina. Ligation of the uterine artery is carried out distal to the vaginal artery and vaginal branches to allow maximal blood circulate to the superior finish of the vagina to facilitate therapeutic. Distension of Vagina 1441 the vagina could be markedly distended, particularly within the area of the posterior a part of the fornix. For example, distension of this part allows palpation of the sacral promontory during a pelvic examination (see the Clinical Box "Pelvic Diameters (Conjugates)"). Lateral distension is restricted by the ischial spines, which project posteromedially, and the sacrospinous ligaments extending from these spines to the lateral margins of the sacrum and coccyx. Digital Pelvic Examination 1443 Because of its comparatively skinny, distensible partitions and central location within the pelvis, the cervix, ischial spines, and sacral promontory could be palpated with the gloved digits in the vagina and/or rectum (manual pelvic examination). Pulsations of the uterine arteries may also be felt through the lateral parts of the fornix, as could irregularities of the ovaries, corresponding to cysts. Radiation therapy for pelvic cancer, surgical problems, and inflammatory bowel disease or diverticulitis may influence the vagina. These insults could type or subsequently develop into abnormal passages (fistulas) between the vaginal lumen and the lumina of the adjoining bladder, ureter, urethra, bowel, or rectum. Urine enters the vagina from vesicovaginal, ureterovaginal, and urethrovaginal fistulas. Flow is continuous from vesico- and ureterovaginal fistulas however occurs only throughout micturition from urethrovaginal fistulas. Culdocentesis A pelvic abscess within the recto-uterine pouch could be drained through an incision made within the posterior part of the vaginal fornix [culdocentesis-"culdo-" referencing the time period "cul-de-sac," a term used traditionally for the recto-uterine pouch (of Douglas)]. Laparoscopic Examination of Pelvic Viscera Visual examination of the pelvic viscera is particularly useful in diagnosing many situations affecting the pelvic viscera, corresponding to ovarian cysts and tumors, endometriosis (the presence of functioning endometrial tissue outdoors the uterus), and ectopic pregnancies. Laparoscopy involves inserting a laparoscope into the peritoneal cavity by way of a small (approximately 2-cm) incision below the umbilicus. Insufflation of carbon dioxide creates a pneumoperitoneum to provide house to visualize, and the pelvis is elevated in order that gravity will pull the intestines into the abdomen. The uterus can be 1447 externally manipulated to facilitate visualization, or further openings (ports) can be made to introduce different devices for manipulation or to allow therapeutic procedures. Anesthesia for Childbirth Several choices can be found to ladies to reduce the ache and discomfort experienced during childbirth. General anesthesia renders the mom unconscious; she is unaware of the labor and supply. Clinicians monitor and regulate maternal respiration and both maternal and fetal cardiac operate.
Order nosipren 40 mg visa
If the S1 nerve root is injured or compressed allergy jewelry buy 20 mg nosipren visa, the ankle reflex is virtually absent allergy testing vic melbourne cheap nosipren 40 mg without prescription. Absence of Plantarflexion If the muscle tissue of the calf are paralyzed, the calcaneal tendon is ruptured, or normal push off is painful, a a lot less efficient and environment friendly push off (from the midfoot) can still be completed by the actions of the gluteus maximus and hamstrings in extending the thigh at the hip joint and the quadriceps in extending the knee. Gastrocnemius Strain 1744 Gastrocnemius strain (tennis leg) is a painful acute injury ensuing from partial tearing of the medial stomach of the gastrocnemius at or close to its musculotendinous junction, often seen in individuals older than 40 years of age. It is attributable to overstretching the muscle by concomitant full extension of the knee and dorsiflexion of the ankle joint. Usually, an abrupt onset of stabbing pain is adopted by edema and spasm of the gastrocnemius. Calcaneal Bursitis Calcaneal bursitis (retro-Achilles bursitis) results from inflammation of the deep bursa of the calcaneal tendon, located between the calcaneal tendon and the superior part of the posterior surface of the calcaneus. Calcaneal bursitis causes pain posterior to the heel and occurs generally during long-distance operating, basketball, and tennis. It is caused by excessive friction on the bursa because the tendon continuously slides over it. Venous Return From Leg 1745 A venous plexus deep to the triceps surae is involved within the return of blood from the leg. When an individual is standing, the venous return from the leg relies upon largely on the muscular activity of the triceps surae (see "Venous Drainage of Lower Limb" on this chapter). The musculovenous pump is improved by the deep fascia that invests the muscular tissues like an elastic stocking. The accent muscle usually appears as a distal belly medial to the calcaneal tendon. Posterior Tibial Pulse the posterior tibial pulse can often be palpated between the posterior floor 1747 of the medial malleolus and the medial border of the calcaneal tendon. Palpation of the posterior tibial pulses is essential for inspecting patients with occlusive peripheral arterial disease. Although posterior tibial pulses are absent in roughly 15% of normal young people, absence of posterior tibial pulses is an indication of occlusive peripheral arterial disease in individuals older than 60 years. For instance, intermittent claudication, characterised by leg ache and cramps, develops throughout strolling and disappears after relaxation. These situations outcome from ischemia of the leg muscular tissues caused by narrowing or occlusion of the leg arteries. Anterior compartment of leg: the anterior compartment, confined by principally unyielding bones and membranes, is vulnerable to compartment syndromes. Lateral compartment of leg: the small lateral compartment accommodates the primary evertors of the foot and the superficial fibular nerve that supplies them. Posterior compartment of leg: the posterior or plantarflexor compartment is subdivided by the transverse intermuscular septum into superficial and deep subcompartments. The ankle refers to the narrowest and malleolar parts of the distal leg, proximal to the dorsum and heel of the foot, together with the ankle joint. The foot, distal to the ankle, offers a platform for supporting the physique when standing and has an essential role in locomotion. The foot and its bones could also be thought-about when it comes to three anatomical and functional zones. The disposition of the bones of the foot and the superior and inferior extensor and fibular retinacula relative to surface options are demonstrated. Skin and Fascia of Foot Marked variations happen in the thickness (strength) and texture of skin, subcutaneous tissue (superficial fascia), and deep fascia in relationship to weight bearing and distribution, ground contact (grip, abrasion), and the necessity for containment or compartmentalization. The subcutaneous tissue is loose deep to the dorsal skin; due to this fact, edema (swelling) is most marked over this floor, particularly anterior to and across the medial malleolus. The skin over the main weight-bearing areas of the sole-the heel, lateral margin, and ball of the foot-is thick. The subcutaneous tissue within the sole is extra fibrous than in other areas of the foot. The pores and skin ligaments additionally anchor the skin to the underlying deep fascia (plantar aponeurosis), enhancing the "grip" of the sole. The skin of the only real is hairless and sweat glands are numerous; the entire sole is sensitive ("ticklish"), especially the thinner-skinned area underlying the arch of the foot. Over the lateral and posterior aspects of the foot, the deep fascia is steady with the plantar fascia, the deep fascia of the sole. The pores and skin and subcutaneous tissue have been eliminated to reveal the deep fascia of the leg and dorsum of the foot. The deep plantar fascia consists of the thick plantar aponeurosis and the thinner medial and lateral plantar fascia. Thinner components of the plantar fascia have been removed, revealing the plantar digital vessels and nerves. The bones and muscle tissue of the foot are surrounded by the deep dorsal and plantar fascia. A large central and smaller medial and lateral compartments of the only real are created by intermuscular septa that stretch deeply from the plantar aponeurosis. The thick, central part of the plantar fascia forms the sturdy plantar aponeurosis, longitudinally organized bundles of dense fibrous connective tissue 1752 investing the central plantar muscle tissue. It resembles the palmar aponeurosis of the palm of the hand however is tougher, denser, and elongated. The plantar fascia holds the elements of the foot together, helps defend the only from damage, and helps to help the longitudinal arches of the foot. The plantar aponeurosis arises posteriorly from the calcaneus and functions like a superficial ligament. Distally, the longitudinal bundles of collagen fibers of the aponeurosis divide into 5 bands that become steady with the fibrous digital sheaths that enclose the flexor tendons that cross to the toes. At the anterior end of the sole, inferior to the heads of the metatarsals, the aponeurosis is bolstered by transverse fibers forming the superficial transverse metatarsal ligament. In the midfoot and forefoot, vertical intermuscular septa prolong deeply (superiorly) from the margins of the plantar aponeurosis towards the first and 5th metatarsals, forming the three compartments of the sole. The medial compartment of the sole is covered superficially by thinner medial plantar fascia. It incorporates the abductor hallucis, flexor hallucis brevis, the tendon of the flexor hallucis longus, and the medial plantar nerve and vessels. The central compartment of the sole is roofed superficially by the dense plantar aponeurosis. It contains the flexor digitorum brevis; the tendons of the flexor hallucis longus and flexor digitorum longus, plus the muscle tissue related to the latter; the quadratus plantae and lumbricals, and the adductor hallucis. The lateral compartment of the only real is covered superficially by the thinner lateral plantar fascia and incorporates the abductor and flexor digiti minimi brevis. In the forefoot solely, a fourth compartment, the interosseous compartment of the foot, is surrounded by the plantar and dorsal interosseous fascias. It incorporates the metatarsals, the dorsal and plantar interosseous muscle tissue, and the deep plantar and metatarsal vessels.
Nosipren 40 mg mastercard
The paroxysms are often set off by touching the face allergy xanax nosipren 10 mg order visa, brushing the enamel allergy journal 5 mg nosipren purchase amex, shaving, consuming, or chewing. The pain is often initiated by touching an particularly delicate set off zone, frequently located around the tip of the nose or the cheek (Haines, 2013). In most cases, that is attributable to pressure of a small aberrant artery (Kiernan, 2013). Other scientists imagine the condition is attributable to a pathological course of affecting neurons within the trigeminal ganglion. The simplest surgical procedure is avulsion or chopping of the branches of the nerve on the infra-orbital foramen. Other treatments have used radiofrequency selective ablation of elements of the trigeminal ganglion by a needle electrode passing through the cheek and foramen ovale. To forestall regeneration of nerve fibers, the sensory root of the trigeminal nerve may be partially reduce between the ganglion and the brainstem (rhizotomy). This loss of sensation might annoy the patient, who may not acknowledge the presence of meals on the lip and cheek or really feel it throughout the mouth on the aspect of the nerve part. Lesions of Trigeminal Nerve Lesions of the complete trigeminal nerve cause widespread anesthesia involving the: Corresponding anterior half of the scalp. Face (except for pores and skin over the angle of the mandible) and the cornea and conjunctiva. Herpes Zoster Infection of Trigeminal Ganglion A herpes zoster virus infection could produce a lesion in the cranial ganglia. Involvement of the trigeminal ganglion occurs in roughly 20% of cases (Mukerji et al. The infection is characterised by an eruption of groups of vesicles following the course of the affected nerve. Usually, the cornea is concerned, often resulting in painful corneal ulceration and subsequent scarring of the cornea. The person is asked if one facet feels the same as or totally different from the other aspect. The testing might then be repeated utilizing warm or chilly instruments and the mild touch of a sharp pin, once more alternating sides. Injuries to Facial Nerve Injury to branches of the facial nerve causes paralysis of the facial muscles (Bell palsy), with or with out lack of taste on the anterior two thirds of the tongue or altered secretion of the lacrimal and salivary glands (see the clinical field "Paralysis of Facial Muscles,"). The most common nontraumatic explanation for facial paralysis is irritation of the facial nerve near the stylomastoid foramen. If the nerve is completely sectioned, the possibilities of complete or even partial recovery are distant. Muscular movement often improves when the nerve damage is associated with blunt head trauma; nevertheless, recovery is most likely not full (Russo et al. However, it often follows publicity to cold, as happens when using in a automotive with a window open. Facial paralysis could additionally be a complication of surgery; consequently, identification of the facial nerve and its branches is important during surgery. The consequences of such paralyses are mentioned in the clinical box "Paralysis of Facial Muscles. In lacerations of the lip, pressure have to be applied on either side of the cut to stop the bleeding. Pulses of Arteries of Face and Scalp the pulses of the superficial temporal and facial arteries may be used for taking the heartbeat. For example, anesthesiologists at the head of the operating desk usually take the temporal pulse the place the superficial temporal artery crosses the zygomatic course of just anterior to the auricle. Clench your teeth and palpate the facial pulse because the facial artery crosses the inferior border of the mandible immediately anterior to the masseter muscle. Stenosis of Internal Carotid Artery At the medial angle of the eye, an anastomosis happens between the facial artery, a department of the exterior carotid artery, and cutaneous branches of the internal carotid artery. With advancing age, the internal carotid artery may become slender (stenotic) owing to atherosclerotic thickening of the intima (innermost coat) of the arteries. Because of the arterial anastomosis, intracranial constructions such as the mind can obtain blood from the connection of the facial artery to the dorsal nasal department of the ophthalmic artery. These wounds bleed profusely because the arteries coming into the periphery of the scalp bleed from each ends owing to plentiful anastomoses. Squamous Cell Carcinoma of Lip Squamous cell carcinoma (cancer) of the lip usually entails the decrease lip. Cancer cells from the central part of the lower lip, the ground of the mouth, and the apex of the tongue unfold to the submental lymph nodes, whereas most cancers cells from lateral parts of the lower lip drain to the submandibular lymph nodes. Structure of scalp: the scalp is a somewhat cell gentle tissue mantle overlaying the calvaria. Muscles of face and scalp: the facial muscles play necessary roles because the dilators and sphincters of the portals of the alimentary (digestive), respiratory, and visual systems (oral and palpebral fissures and nostrils), controlling what enters and some of what exits from our our bodies. The terminal branches of the arteries of the face anastomose freely (including anastomoses throughout the midline with their contralateral partners). Thus, bleeding from facial lacerations could additionally be diffuse, with the lacerated vessel bleeding from both ends. Thus, when lacerated, these arteries bleed from each ends, like those of the face, however are less capable of constrict or retract than different superficial vessels; subsequently, profuse bleeding results. The veins of the face and scalp usually accompany arteries, offering a primarily superficial venous drainage. The lymphatic drainage of many of the face follows the venous drainage to lymph nodes across the base of the anterior part of the top (submandibular, parotid, and superficial cervical nodes). The two layers of dura separate to form dural venous sinuses, such because the superior sagittal sinus. Cranial dura mater has two layers, whereas spinal dura mater consists of a single layer. The calvaria has been eliminated to reveal the external (periosteal layer) of the dura mater. On the proper, an angular flap of dura has been turned anteriorly; the convolutions of the cerebral cortex are visible through the arachnoid mater. The inner facet of the calvaria reveals pits (dotted traces, granular foveolae) within the frontal and parietal bones, that are produced by enlarged arachnoid granulations or clusters of smaller ones (as in D). Multiple small emissary veins pass between the superior sagittal sinus and the veins in the diplo� and scalp through small emissary foramina (arrows) positioned on each side of the sagittal suture. The sinuous vascular groove (M) on the lateral wall is fashioned by the frontal branch of the middle meningeal artery. The intermediate and inside layers (arachnoid and pia) are steady membranes that collectively make up the leptomeninx (G.
Nosipren 40 mg buy
The heads come collectively on the inferior margin of the popliteal fossa allergy symptoms burning lips 20 mg nosipren mastercard, the place they type the inferolateral and inferomedial boundaries of this fossa allergy forecast fredericksburg va generic nosipren 5 mg otc. Because its fibers are largely of the white, fast-twitch (type 2) selection, contractions of the gastrocnemius produce fast actions during running and jumping. It features most effectively when the knee is prolonged (and is maximally activated when knee extension is combined with dorsiflexion, as within the dash start). The soleus is positioned deep to the gastrocnemius and is the "workhorse" of plantarflexion. The soleus has a steady proximal attachment in the shape of an inverted U to the posterior elements of the fibula and tibia and a tendinous arch between them, the tendinous arch of soleus (L. The popliteal artery and tibial nerve exit the popliteal fossa by passing by way of this arch, the popliteal artery simultaneously bifurcating into its terminal branches, the anterior and posterior tibial arteries. The soleus can be palpated on all sides of the gastrocnemius when the person is "standing on their toes" (weight on forefoot with ankle plantarflexed, as in. The soleus is thus an antigravity muscle (the predominant plantarflexor for standing and strolling), which contracts antagonistically however cooperatively (alternately) with the dorsiflexor muscles of the leg to preserve 1725 steadiness. This vestigial muscle is absent in 5�10% of individuals and is very variable in size and form when current (most generally a tapering slip concerning the dimension of the small finger). It acts with the gastrocnemius but is insignificant as either a flexor of the knee or a plantarflexor of the ankle. The plantaris has been thought of to be an organ of proprioception for the larger plantarflexors, as it has a excessive density of muscle spindles (receptors for proprioception). The popliteus acts on the knee joint, whereas the opposite muscle tissue plantarflex the ankle with two persevering with on to flex the toes. However, because of their smaller size and the close proximity of their tendons to the axis of the ankle joint, the "nontriceps" plantarflexors collectively produce solely about 7% of the total drive of plantarflexion, and on this, the fibularis longus and brevis are most vital. The foot is raised as within the push off phase of walking, demonstrating the place of the plantarflexor tendons as they cross the ankle. Observe the sesamoid bone appearing as a "foot stool" for the 1st metatarsal, giving it additional height and protecting the flexor hallucis longus tendon. This view demonstrates the disposition of the deep plantarflexor tendons in the sole of the foot. Damage to a number of of the listed spinal wire segments or to the motor nerve roots arising from them results in paralysis of the muscles concerned. The two muscular tissues of the posterior compartment that pass to the toes are crisscrossed-that is, the muscle attaching medially to the nice toe (flexor hallucis longus) arises laterally (from the fibula) within the deep subcompartment, and the muscle attaching to the lateral 4 toes (flexor digitorum longus) arises medially (from the tibia). The popliteus is a thin, triangular muscle that forms the inferior a part of the ground of the popliteal fossa. Proximally, its tendinous attachment to the lateral aspect of the lateral femoral condyle and its broader attachment to the lateral meniscus happen between the fibrous layer and the synovial membrane of the joint capsule of the knee. When standing with the knees locked within the fully extended place, the popliteus acts to rotate the femur laterally 5� on the tibial plateaus, releasing the knee from its close-packed or locked position so that flexion can happen. When the foot is off the ground and the knee is flexed, the popliteus can help the medial hamstrings (the "semi-muscles") in rotating the tibia medially beneath the femoral condyles. When barefoot, this thrust is delivered by the good toe; but with soled sneakers on, it becomes part of the thrust of plantarflexion delivered by the forefoot. The tendon then crosses deep to the tendon of the flexor digitorum longus in the sole of the foot. These bones defend the tendon from the stress of the pinnacle of the first metatarsal bone. While standing (especially on one foot), nevertheless, the 2 muscle tissue could cooperate to depress the lateral side of the foot and pull medially on the leg as wanted to counteract lateral leaning for stability. It runs vertically by way of the popliteal fossa with the popliteal artery, passing between the heads of the gastrocnemius, the two buildings exiting the fossa by passing deep to the tendinous arch of the soleus. Postero-inferior to the medial malleolus, the tibial nerve divides into the medial and lateral plantar nerves. A department of the tibial nerve, the medial sural cutaneous nerve, is often joined by the sural speaking department of the common fibular nerve to type the sural nerve. The sural nerve supplies the pores and skin of the lateral and posterior a part of the inferior third of the leg and the lateral facet of the foot. It begins at the distal border of the popliteus, as the popliteal artery passes deep to the tendinous arch of the soleus and simultaneously bifurcates into its terminal branches. Close to its origin, the posterior tibial artery gives rise to its largest department, the fibular artery, which runs lateral and parallel to it, also inside the deep subcompartment. During its descent, the posterior tibial artery is accompanied by the tibial nerve and veins. Deep to the flexor retinaculum and the origin of the abductor hallucis, the posterior tibial artery divides into medial and lateral plantar arteries, the arteries of the only of the foot. The fibular (peroneal) artery, the most important and most necessary branch of the posterior tibial artery, arises inferior to the distal border of the popliteus and the tendinous arch of the soleus. The fibular artery offers muscular branches to the popliteus and other muscles in each the posterior and the lateral compartments of the leg. Distally, the fibular artery gives rise to a perforating department and terminal lateral malleolar and calcaneal branches. The perforating branch pierces the interosseous membrane and passes to the dorsum of the foot, where it anastomoses with the arcuate artery. The lateral calcaneal branches supply the heel, and the lateral malleolar branch joins other malleolar branches to form a peri-articular arterial anastomosis of the ankle. The circumflex fibular artery arises from the origin of the anterior or posterior tibial artery at the knee and passes laterally over the neck of the fibula to the anastomoses around the knee. It pierces the tibialis posterior, to which it provides branches, and enters the nutrient foramen within the proximal third of the posterior surface of the tibia. Surface Anatomy of Leg the tibial tuberosity is an simply palpable elevation on the anterior side of the proximal part of the tibia, roughly 5 cm distal to the apex of the patella. This oval elevation signifies the level of the top of the fibula and the bifurcation of the popliteal artery into the anterior and posterior tibial arteries. Extensors and flexors of toes are being contracted simultaneously, demonstrating extensor tendons without elevating toes from floor. The patellar ligament may be felt as it extends from the inferior border of the 1734 apex of the patella. When the knee flexes to a proper angle, a depression could additionally be felt on each side of the patellar ligament. The head of the fibula is subcutaneous and may be palpated on the posterolateral aspect of the knee, on the degree of the tibial tuberosity. The tendon of the biceps femoris could additionally be traced by palpating its distal attachment to the lateral side of the top of the fibula.
10 mg nosipren generic visa
Both kinds of pulmonary stenoses produce a restriction of proper ventricular outflow and should happen collectively allergy medicine orange juice generic nosipren 20 mg amex. An incompetent pulmonary valve ends in a backrush of blood under excessive strain into the proper ventricle during diastole allergy medicine decongestant discount nosipren 20 mg without prescription. Pulmonic regurgitation could also be heard through a stethoscope as a coronary heart murmur, an irregular sound from the center, produced on this case by damage to the cusps of the pulmonary valve. Aortic Valve Stenosis Aortic valve stenosis is probably the most frequent valve abnormality. For these born in the early- and mid20th century, rheumatic fever was a typical trigger however now accounts for <10% of cases of aortic stenosis. The great majority of aortic stenoses is a result of degenerative calcification and involves medical consideration within the sixth decade of life or later. Aortic stenosis causes extra work for the heart, resulting in left ventricular hypertrophy. Aortic Valve Insufficiency Insufficiency of the aortic valve leads to aortic regurgitation (backrush of blood into the left ventricle), producing a heart murmur and a collapsing pulse (forcible impulse that quickly diminishes). Echocardiography Echocardiography (ultrasonic cardiography) is a technique of graphically recording the position and motion of the heart by the echo obtained from beams of ultrasonic waves directed by way of the thoracic wall. This approach may detect as little as 20 mL of fluid within the pericardial cavity, similar to that resulting from pericardial effusion. Doppler echocardiography is a way that demonstrates and records the move of blood via the center and nice vessels by Doppler ultrasonography, making it especially helpful in the diagnosis and evaluation of problems with blood flow through the center, such as septal defects, and in delineating valvular stenosis and regurgitation, especially on the left side of the guts. Sonographer placing transducer in a left intercostal space in the parasternal line, overlying the heart. Coronary Angiography Using standard coronary angiography, the coronary arteries may be visualized with coronary arteriograms. A lengthy, slim catheter is passed into the ascending aorta through the femoral artery within the inguinal area. Under fluoroscopic management, the tip of the catheter is positioned just inside the opening of a coronary artery. A small injection of radiopaque distinction material 904 is made, and cineradiographs are taken to present the lumen of the artery and its branches, in addition to any stenotic areas which may be present. It has many causes, all of which end in a lowered blood provide to the vital 905 myocardial tissue. The three most common sites of coronary artery occlusion and the proportion of occlusions involving each artery are. The most typical cause of ischemic coronary heart disease is coronary artery insufficiency resulting from atherosclerosis. Coronary Atherosclerosis the atherosclerotic process, characterized by lipid deposits within the intima (lining layer) of the coronary arteries, begins throughout early adulthood and slowly ends in stenosis of the lumina of the arteries. As coronary atherosclerosis progresses, the collateral channels connecting one coronary artery with the opposite expand, which can initially permit enough perfusion of the guts throughout relative inactivity. Despite this compensatory mechanism, the myocardium might not obtain sufficient oxygen when the heart needs to carry out increased amounts of labor. Slowly Progressive Coronary Artery Disease In slow occlusion of a coronary artery, the collateral circulation has time to increase in order that enough perfusion of the myocardium can happen when a 907 probably ischemic event happens. On sudden blockage of a large coronary department, some infarction might be inevitable, but the extent of the world damaged depends on the diploma of growth of collateral anastomotic channels. If giant branches of both coronary arteries are partially obstructed, an extracardiac collateral circulation could also be used to provide blood to the guts. These collaterals connect the coronary arteries with the vasa vasorum (small arteries) in the tunica adventitia of the aorta and pulmonary arteries and with branches of the internal thoracic, bronchial, and phrenic arteries. Angina Pectoris Pain that originates in the heart is called angina or angina pectoris (L. Individuals with angina generally describe the transient (15 seconds to 15 minutes) but reasonably severe constricting pain as tightness within the thorax, deep to the sternum. The pain is the outcomes of ischemia of the myocardium that falls wanting inducing the mobile necrosis that defines infarction. The decreased blood flow results in less oxygen being delivered to the cardiac striated muscle cells. As a results of the restricted anaerobic metabolism of the myocytes, lactic acid accumulates and the pH is reduced in affected areas of the center. When food enters the stomach, blood circulate to it and other parts of the digestive tract is increased. Sublingual nitroglycerin (medication positioned or sprayed under the tongue for absorption via the oral mucosa) could additionally be administered as a end result of it dilates the coronary (and other) arteries. Furthermore, the dilated vessels accommodate more of the blood quantity, so much less blood arrives within the coronary heart, relieving coronary heart congestion. Coronary Bypass Graft Patients with obstruction of their coronary circulation and extreme angina might endure a coronary bypass graft operation. A segment of an artery or vein is related to the ascending aorta or to the proximal a half of a coronary artery after which to the coronary artery distal to the stenosis. The nice saphenous vein is commonly harvested for coronary bypass surgery because it (1) has a diameter equal to or greater than that of the coronary arteries, (2) could be easily dissected from the lower limb, and (3) and presents comparatively lengthy portions with a minimal occurrence of valves or branching. Reversal of the implanted phase of vein can negate the impact of a valve if a valved phase should be used. A coronary bypass graft shunts blood from the aorta to a stenotic coronary artery to increase the flow distal to the obstruction. Simply said, it supplies a detour across the stenotic space (arterial stenosis) or blockage (arterial atresia). Revascularization of the myocardium can also be achieved by surgically anastomosing an internal thoracic artery with a coronary artery. Hearts with coronary bypass grafts are generally discovered during dissections in the gross anatomy laboratory. Coronary Angioplasty Cardiologists or interventional radiologists use percutaneous transluminal coronary angioplasty in which they cross a catheter with a small inflatable balloon hooked up to its tip into the obstructed coronary artery. The vessel is stretched to improve the dimensions of the lumen, thus enhancing blood flow. In other instances, 910 thrombokinase is injected by way of the catheter; this enzyme dissolves the blood clot. After dilation of the vessel, an intravascular stent could additionally be introduced to preserve the dilation. Intravascular stents are composed of rigid or semirigid tubular meshes, collapsed during introduction. Functional testing of the center contains exercise tolerance tests (treadmill stress tests), primarily to check the implications of attainable coronary artery disease. Exercise tolerance checks are of considerable significance in detecting the cause of heartbeat irregularities. Coronary Occlusion and Conducting System of Heart Damage to the conducting system of the guts, typically resulting from ischemia caused by coronary artery disease, produces disturbances of cardiac muscle contraction.
Generic nosipren 40 mg without prescription
Although mostly 2298 recognized for its role because the phonating mechanism for voice production allergy treatment for 18 month old nosipren 40 mg purchase, its most significant function is to guard the air passages allergy medicine daily 10 mg nosipren order visa, especially during swallowing when it serves as the "sphincter" or "valve" of the decrease respiratory tract, thus sustaining a patent airway. Because the air and food passages share the oropharynx, separation of meals and air should occur to proceed into the trachea (anterior) and esophagus (posterior). The laryngeal skeleton consists of 9 cartilages: three are single (thyroid, cricoid, and epiglottic), and three are paired (arytenoid, corniculate, and cuneiform). The larynx extends vertically from the tip of the heart-shaped epiglottis to the inferior border of the cricoid cartilage. The thyroid cartilage shields the smaller cartilages of the larynx, and the hyoid shields the superior a part of the epiglottic cartilage. The epiglottic cartilage is pitted for mucous glands, and its stalk is attached by the thyro-epiglottic ligament to the angle of the thyroid cartilage superior to the vocal ligaments. The vocal ligament, which forms the skeleton of the vocal fold, extends from the vocal means of the arytenoid cartilage to the "angle" of the thyroid cartilage, and there joins its fellow inferior to the thyro-epiglottic ligament. The thyroid cartilage is the largest of the cartilages; its superior border lies opposite the C4 vertebra. The inferior two thirds of its two plate-like laminae fuse anteriorly in the median plane to type the laryngeal prominence. Superior to this prominence, the laminae diverge to form a Vshaped superior thyroid notch. The less distinct inferior thyroid notch is a shallow indentation in the course of the inferior border of the cartilage. The posterior border of each lamina tasks superiorly as the superior horn and inferiorly because the inferior horn. The thick median a part of this membrane is the median thyrohyoid ligament; its lateral parts are the lateral thyrohyoid ligaments. The inferior horns articulate with the lateral surfaces of the cricoid cartilage on the cricothyroid joints. The main movements at these joints are rotation and gliding of the thyroid cartilage, which end in adjustments in the length of the vocal folds. The cricoid cartilage is shaped like a signet ring with its band facing anteriorly. The posterior (signet) part of the cricoid is the lamina, and the anterior (band) half is the arch. Although much smaller than the thyroid cartilage, the cricoid cartilage is thicker and stronger and is the one complete ring of cartilage to encircle any a half of the airway. It attaches to the inferior margin of 2301 the thyroid cartilage by the median cricothyroid ligament and to the primary tracheal ring by the cricotracheal ligament. Where the larynx is closest to the skin and most accessible, the median cricothyroid ligament could additionally be felt as a soft spot during palpation inferior to the thyroid cartilage. The arytenoid cartilages are paired, three-sided pyramidal cartilages that articulate with the lateral components of the superior border of the cricoid cartilage lamina. Each cartilage has an apex superiorly, a vocal course of anteriorly, and a large muscular course of that projects laterally from its base. The vocal course of provides the posterior attachment for the vocal ligament, and the muscular process serves as a lever to which the posterior and lateral cricoarytenoid muscle tissue are attached. The crico-arytenoid joints, situated between the bases of the arytenoid cartilages and the superolateral surfaces of the lamina of the cricoid cartilage. These movements are important in approximating, tensing, and stress-free the vocal folds. The elastic vocal ligaments lengthen from the junction of the laminae of the thyroid cartilage anteriorly to the vocal strategy of the arytenoid cartilage posteriorly. These ligaments are the thickened, free superior border of the conus elasticus or cricovocal membrane. The elements of the membrane extending laterally between the vocal folds and the superior border of the cricoid are the lateral cricothyroid ligaments. The fibro-elastic conus elasticus blends anteriorly with the median cricothyroid ligament. The conus elasticus and overlying mucosa shut the tracheal inlet aside from the central rima glottidis (opening between the vocal folds). The epiglottic cartilage, consisting of elastic cartilage, gives flexibility to the epiglottis, a heart-shaped cartilage lined with mucous membrane. Situated posterior to the foundation of the tongue and the hyoid and anterior to the laryngeal inlet, the epiglottic cartilage forms the superior a part of the anterior wall and the superior margin of the inlet. Its tapered inferior end, the stalk of the epiglottis, is attached to the angle fashioned by the thyroid laminae by the thyro-epiglottic ligament. The hyo-epiglottic ligament attaches the anterior floor of the epiglottic cartilage to the hyoid. Its free inferior margin constitutes the vestibular ligament, which is covered loosely by mucosa to form the vestibular fold. This fold lies superior to the vocal fold and extends from the thyroid cartilage to the arytenoid cartilage. The free superior margin of the quadrangular membrane forms the aryepiglottic ligament, which is covered with mucosa to kind the aryepiglottic fold. The corniculate and cuneiform cartilages appear as small nodules in the posterior part of the aryepiglottic folds. The quadrangular membrane and conus elasticus are the superior and inferior elements of the submucosal fibro-elastic membrane of the larynx. The epiglottis is a leaf-shaped plate of elastic fibrocartilage, which is covered with mucous membrane (pink) and is attached anteriorly to the hyoid by the hyo-epiglottic ligament (gray). The epiglottis serves as a diverter valve over the superior aperture of the larynx throughout swallowing. The posterior wall of the larynx is split within the median plane, and the two sides are spread apart and held in place by a surgical needle. On the proper side, the mucous and submucous coats are peeled off, and the skeletal coat- consisting of cartilages, ligaments, and the fibro-elastic membrane-is uncovered. The laryngeal cavity extends from the laryngeal inlet, via which it communicates with the laryngopharynx, to the extent of the inferior border of the cricoid cartilage. This coronal section shows the compartments of the larynx: the vestibule, center compartment with left and right ventricles, and the infraglottic cavity. The laryngeal inlet is bounded (1) anteriorly by the free curved fringe of the epiglottis; (2) posteriorly by the arytenoid cartilages, the corniculate cartilages that cap them, and the interarytenoid fold that unites them; and (3) on both sides by the aryepiglottic fold that contains the superior finish of the cuneiform cartilage. The planes of these transverse studies, oriented in the same path as part (C), move superior (D) and inferior (E) to the rima glottidis. The 2306 shape of the rima glottidis, the aperture between the vocal folds, varies according to the place of the vocal folds. During a deep inhalation, the vocal ligaments are abducted by contraction of the posterior crico-arytenoid muscular tissues, opening the rima glottidis extensively into an inverted kite form. Stronger contraction of the same muscle tissue seals the rima glottidis (Valsalva maneuver). During whispering, the vocal ligaments are strongly adducted by the lateral crico-arytenoid muscles, however the relaxed arytenoid muscular tissues permit air to cross between the arytenoid cartilages (intercartilaginous part of rima glottidis), which is modified into toneless speech.
Nosipren 40 mg discount without a prescription
Adductors and abductors: these muscle tissue transfer the vocal folds to open and close the rima glottidis allergy testing lincoln ne 10 mg nosipren sale. The principal adductors are the lateral crico2310 arytenoid muscles allergy symptoms to kiwi fruit 40 mg nosipren cheap visa, which pull the muscular processes anteriorly, rotating the arytenoid cartilages in order that their vocal processes swing medially. When this motion is combined with that of the transverse and indirect arytenoid muscles, which pull the arytenoid cartilages together, air pushed through the rima glottidis causes vibrations of the vocal ligaments (phonation). This is the place of whispering when the breath is modified into voice in the absence of tone. Sphincters: the mixed actions of most of the muscle tissue of the laryngeal inlet result in a sphincteric motion that closes the laryngeal inlet as a protecting mechanism throughout swallowing. Contraction of the lateral cricoarytenoids, transverse and indirect arytenoids, and aryepiglottic muscle tissue brings the aryepiglottic folds together and pulls the arytenoid cartilages towards the epiglottis. This motion happens reflexively in response to the presence of liquid or particles approaching or within the laryngeal vestibule. It is perhaps our strongest reflex, diminishing solely after loss of consciousness, as in drowning. Tensors: the principal tensors are the cricothyroid muscle tissue, which tilt or pull the prominence or angle of the thyroid cartilage anteriorly and inferiorly toward the arch of the cricoid cartilage. This increases the space between the thyroid prominence and the arytenoid cartilages. Because the anterior ends of the vocal ligaments connect to the posterior side of the prominence, the vocal ligaments elongate and tighten, raising the pitch of the voice. Relaxers: the principal muscle tissue in this group are the thyro-arytenoid muscle tissue, which pull the arytenoid cartilages anteriorly, toward the thyroid angle (prominence), thereby stress-free the vocal ligaments to lower the pitch of the voice. The vocalis muscles lie medial to the thyro-arytenoid muscle tissue and lateral to the vocal ligaments inside the vocal folds. The vocalis muscular tissues produce minute adjustments of the vocal ligaments, selectively tensing and relaxing the anterior and posterior components, respectively, of the vocal folds throughout animated speech and singing. The laryngeal arteries, branches of the superior and inferior thyroid arteries, supply the larynx. The superior laryngeal 2311 artery accompanies the inner department of the superior laryngeal nerve via the thyrohyoid membrane and branches to supply the inner surface of the larynx. The cricothyroid artery, a small branch of the superior thyroid artery, supplies the cricothyroid muscle. The inferior laryngeal artery, a department of the inferior thyroid artery, accompanies the inferior laryngeal nerve (terminal a part of the recurrent laryngeal nerve) and provides the mucous membrane and muscles within the inferior a part of the larynx. The superior and inferior thyroid arteries give rise to the superior and inferior laryngeal arteries, respectively; they anastomose with one another. The inferior laryngeal vein joins the inferior thyroid vein or the venous plexus of veins on the anterior side of the trachea, which empties into the left brachiocephalic vein. The laryngeal lymphatic vessels superior to the vocal folds accompany the superior laryngeal artery through the thyrohyoid membrane and drain into the superior deep cervical lymph nodes. The lymphatic vessels inferior to the vocal folds drain into the pretracheal or paratracheal lymph nodes, which drain into the inferior deep cervical lymph nodes. The superior laryngeal nerve arises from the inferior vagal ganglion on the superior end of the carotid triangle. The nerves of the larynx are the inner and external branches of the superior laryngeal nerve and the inferior laryngeal nerve from the recurrent laryngeal nerve. The proper recurrent laryngeal nerve passes inferior to the right subclavian artery. The internal laryngeal nerve, the larger of the terminal branches of the superior laryngeal nerve, pierces the thyrohyoid membrane with the superior laryngeal artery, supplying sensory fibers to the laryngeal mucous membrane of the laryngeal vestibule and middle laryngeal cavity, including the superior floor of the vocal folds. The exterior laryngeal nerve, the smaller terminal 2314 department of the superior laryngeal nerve, descends posterior to the sternothyroid muscle in company with the superior thyroid artery. At first, the external laryngeal nerve lies on the inferior pharyngeal constrictor; it then pierces the muscle, contributing to its innervation (with the pharyngeal plexus), and continues to supply the cricothyroid muscle. The inferior laryngeal nerve, the continuation of the recurrent laryngeal nerve (a branch of the vagus nerve), enters the larynx by passing deep to the inferior border of the inferior pharyngeal constrictor and medial to the lamina of the thyroid cartilage. It divides into anterior and posterior branches, which accompany the inferior laryngeal artery into the larynx. The posterior branch provides the posterior crico-arytenoid and transverse and indirect arytenoid muscles. Because it supplies all the intrinsic muscles except the cricothyroid, the inferior laryngeal nerve is the first motor nerve of the larynx. However, it additionally supplies sensory fibers to the mucosa of the infraglottic cavity. It transports air to and from the lungs, and its epithelium propels debris-laden mucus toward the pharynx for expulsion from the mouth. The trachea is a fibrocartilaginous tube, supported by incomplete cartilaginous tracheal cartilages (rings), that occupies a median position within the neck. The posterior gaps in the tracheal rings are spanned by the involuntary trachealis muscle, smooth muscle connecting the ends of the rings. The trachea extends from the inferior end of the larynx at the level of the C6 vertebra. Lateral to the trachea are the common carotid arteries and the lobes of the thyroid gland. Inferior to the isthmus of the thyroid gland are the jugular venous arch and the inferior thyroid veins. The brachiocephalic trunk is expounded to the best facet of the trachea in the root of the neck. Deviation of the trachea from the midline, apparent superficially or radiographically, often alerts the presence of a pathological course of. Alimentary Layer of Cervical Viscera In the alimentary layer, cervical viscera participate in the digestive capabilities of the physique. Although the pharynx conducts air to the larynx, trachea, and lungs, the pharyngeal constrictors direct (and the epiglottis deflects) meals to the esophagus. The esophagus, also involved in meals propulsion, is the beginning of the alimentary canal (digestive tract). The pharynx extends from the cranial base to the inferior border of the cricoid cartilage anteriorly and the inferior border of the C6 vertebra posteriorly. The flat posterior wall of the pharynx lies in opposition to the prevertebral 2317 layer of deep cervical fascia. Openings within the anterior wall communicate with the nasal, oral, and laryngeal cavities. On each side of the laryngeal inlet, separated from it by the aryepiglottic fold, a piriform fossa (recess) is shaped by the invagination of the larynx into the anterior wall of the laryngopharynx.