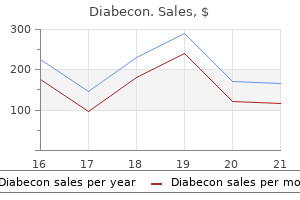
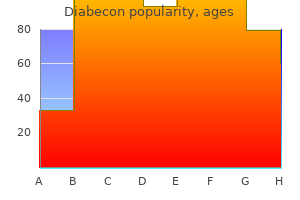
Diabecon dosages: 60 caps
Diabecon packs: 1 bottles, 2 bottles, 3 bottles, 4 bottles, 5 bottles, 6 bottles, 7 bottles, 8 bottles, 9 bottles, 10 bottles
Buy cheap diabecon 60 caps
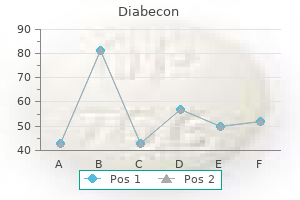
It is bounded superiorly by the xiphoid process and costal margins diabetes symptoms sweet taste in mouth buy 60 caps diabecon, posteriorly by the vertebral column diabetes chart purchase 60 caps diabecon with amex, and inferiorly by the higher parts of the pelvic bones. It is often a single layer just like, and steady with, the tremendous cial fascia throughout different regions of the body. However, in the decrease region of the anterior a part of the abdominal wall, below the umbilicus, it types two layers: a super cial fatty layer and a deeper membranous layer. It is steady over the inguinal ligament with the supercial fascia of the thigh and with an analogous layer within the perineum. In males, this tremendous cial layer continues over the penis and, after dropping its fats and fusing with the deeper layer of super cial fascia, continues into the scrotum the place it forms a specialized fascial layer containing smooth muscle bers (the dartos fascia). In ladies, this tremendous cial layer retains some fats and is a part of the labia majora. Inferiorly, it continues into the thigh, but slightly below the inguinal ligament, it fuses with the deep fascia of the thigh (the fascia lata;. In men, the deeper membranous layer of super cial fascia blends with the tremendous cial layer as they both move over the penis, forming the tremendous cial fascia of the penis, earlier than they continue into the scrotum where they type the dartos fascia. Also in men, extensions of the deeper membranous layer of super cial fascia hooked up to the pubic symphysis pass inferiorly onto the dorsum and sides of the penis to type the fundiform ligament of the penis. In girls, the membranous layer of the tremendous cial fascia continues into the labia majora and the anterior a half of the perineum. Anterolateral muscular tissues There are ve muscular tissues within the anterolateral group of abdominal wall muscular tissues (Table 4. Each of those ve muscle tissue has speci c actions, but collectively the muscle tissue are important: for the maintenance of many regular physiological features, to maintain the abdominal viscera throughout the abdominal cavity, to shield the viscera from injury, and to help preserve the position of the viscera within the erect posture against the motion of gravity. Contraction of those muscular tissues assists in each quiet and compelled expiration by pushing the viscera upward (which helps push the relaxed diaphragm farther into the thoracic cavity) and in coughing and vomiting. All these muscle tissue are also concerned in any motion that increases intra-abdominal strain, including parturition (childbirth), micturition (urination), and defecation (expulsion of feces from the rectum). Latis s imus dors i mus cle Abdominal part of pectoralis major mus cle Linea alba External oblique mus cle Aponeuros is of exterior oblique Inguinal ligament Anterior s uperior iliac s pine. External oblique Anterior s uperior Aponeuros is of iliac s pine exterior indirect Flat muscular tissues External oblique essentially the most tremendous cial of the three at muscles within the anterolateral group of abdominal wall muscular tissues is the external oblique, which is instantly deep to the tremendous cial fascia (Table four. Its laterally placed muscle bers pass in an inferomedial course, while its large aponeurotic element covers the anterior part of the abdominal wall to the midline. Approaching the midline, the aponeuroses are entwined, forming the linea alba, which extends from the xiphoid process to the pubic symphysis. Associated ligaments the decrease border of the external indirect aponeurosis forms the inguinal ligament on all sides. This thickened reinforced free edge of the exterior indirect aponeurosis passes between the anterior superior iliac spine laterally and the pubic tubercle medially. It folds under itself forming a trough, which performs an essential position within the formation of the inguinal canal. Several different ligaments are also shaped from extensions of the bers on the medial end of the inguinal ligament: the lacunar ligament is a crescent-shaped extension of bers at the medial finish of the inguinal ligament Inguinal ligament Lacunar ligament Pubic tubercle Femoral artery and vein. It crosses the midline anteriorly, associating with the transversalis fascia of the alternative facet, and is continuous with the fascia on the inferior floor of the diaphragm. It is steady posteriorly with the deep fascia masking the muscle tissue of the posterior stomach wall and attaches to the thoracolumbar fascia. After attaching to the crest of the ilium, the transversalis fascia blends with the fascia covering the muscular tissues related to the higher regions of the pelvic bones and with similar fascia overlaying the muscular tissues of the pelvic cavity. Internal oblique Deep to the exterior indirect muscle is the inner indirect muscle, which is the second of the three at muscle tissue (Table 4. This muscle is smaller and thinner than the external indirect, with most of its muscle bers passing in a superomedial path. Its lateral muscular parts end anteriorly as an aponeurosis that blends into the linea alba at the midline. Transversus abdominis Vertical muscle tissue the 2 vertical muscular tissues in the anterolateral group of belly wall muscles are the large rectus abdominis and the small pyramidalis (Table 4. It ends in an anterior aponeurosis, which blends with the linea alba at the midline. Rectus abdominis Transversalis fascia Each of the three at muscle tissue is covered on its anterior and posterior surfaces by a layer of deep (or investing) fascia. In common, these layers are unremarkable aside from the layer deep to the transversus abdominis muscle (the transversalis fascia), which is best developed. The transversalis fascia is a continuous layer of deep fascia that lines the abdominal cavity and continues into the rectus abdominis is a protracted, at muscle and extends the length of the anterior stomach wall. It is a paired muscle, separated in the midline by the linea alba, and it widens and thins as it ascends from the pubic symphysis to the costal margin. This small, triangular muscle, which can be absent, is anterior to the rectus abdominis, has its base on the pubis, and its apex is connected superiorly and medially to the linea alba. Pectineal line External oblique mus cle Rib X Inguinal ligament Internal indirect mus cle and aponeuros is Anterior s uperior iliac s pine Pubic tubercle Lacunar ligament Linea alba Aponeuros is of exterior oblique Pubic s ymphys is 138. Regional anatomy � Abdominal wall four External oblique mus cle Rib X Trans vers us abdominis mus cle and aponeuros is Anterior s uperior iliac s pine Aponeuros is of exterior oblique Aponeuros is of internal oblique Linea alba External indirect mus cle Rectus abdominis mus cle Tendinous inters ection Pos terior wall of rectus s heath Internal indirect mus cle Arcuate line Trans vers alis fas cia Linea alba Pyramidalis mus cle. Rectus sheath the rectus abdominis and pyramidalis muscular tissues are enclosed in an aponeurotic tendinous sheath (the rectus sheath) formed by a singular layering of the aponeuroses of the external and inside indirect, and transversus abdominis muscles. The rectus sheath completely encloses the higher threequarters of the rectus abdominis and covers the anterior floor of the decrease one-quarter of the muscle. As no sheath covers the posterior surface of the decrease quarter of the rectus abdominis muscle, the muscle at this level is in direct contact with the transversalis fascia. The formation of the rectus sheath surrounding the higher three-quarters of the rectus abdominis muscle has the next pattern: the anterior wall consists of the aponeurosis of the external oblique and half of the aponeurosis of the interior oblique, which splits at the lateral margin of the rectus abdominis. Containing varying amounts of fat, this layer not only strains the stomach cavity but is also steady with a similar layer lining the pelvic cavity. It is plentiful on the posterior abdominal wall, particularly across the kidneys, continues over organs coated by peritoneal re ections, and, as the vasculature is situated in this layer, extends into mesenteries with the blood vessels. The fascia toward the anterior side of the body is described as preperitoneal (or, less Extraperitoneal fas cia. The posterior wall of the rectus sheath consists of the opposite half of the aponeurosis of the interior indirect and the aponeurosis of the transversus abdominis. Preperitoneal Retroperitoneal At a degree midway between the umbilicus and the pubic symphysis, similar to the beginning of the decrease one-fourth of the rectus abdominis muscle, the entire aponeuroses transfer anterior to the rectus muscle. From this level inferiorly, the rectus abdominis muscle is in direct contact with the transversalis fascia. Extraperitoneal fascia a hundred and forty Deep to the transversalis fascia is a layer of connective tissue, the extraperitoneal fascia, which separates the.
Diabecon 60 caps purchase with amex
Parental presence throughout induction of anesthesia versus sedative premedication: Which intervention is more practical Practice guidelines for perioperative blood management: An up to date report by the American Society of Anesthesiologists Task Force on Perioperative Blood Management diabetes diet how many carbs 60 caps diabecon. Blood loss blood sugar equipment order diabecon 60 caps on line, alternative, and associated morbidity in infants and youngsters undergoing craniofacial surgery. Anesthesia-related cardiac arrest in youngsters: Update from the Pediatric Perioperative Cardiac Arrest Registry. Red blood cell transfusion threshold in postsurgical pediatric intensive care sufferers: a randomized scientific trial. Clinical practice guideline: Polysomnography for sleepdisordered respiration prior to tonsillectomy in kids. Perioperative danger factors for antagonistic airway occasions in sufferers present process cleft palate repair. Anesthetic management of patients with an anterior mediastinal mass: Continuing skilled improvement. A prospective cohort examine of emergence agitation in the pediatric postanesthesia care unit. A 2-year-old woman is scheduled for emergency exploratory laparotomy for intestinal obstruction. Succinylcholine could additionally be used if preceded by a nondepolarizing neuromuscular blocker. How a lot fluid (approximately) ought to she receive during her first hour of surgery As the pediatric postanesthesia care unit resident, which of these sufferers has the best danger of postoperative apnea A 2-year-old following elective setting of an arm fracture 2 weeks after an upper respiratory infection 5. Which of the following will trigger the best issue in successfully passing a nasotracheal tube in a 1-month-old youngster As in comparability with a standard adult, the oxygen consumption (cc/kg basis) of the neonate is: A. Which of the next best reflects electrolyte and acid-base abnormalities seen in the neonate with pyloric stenosis Potassium Acid Base Chloride Diagnosis Metabolic alkalosis Metabolic acidosis Metabolic acidosis Respiratory alkalosis 8. Which of the next represents the conventional blood gasoline values for a full-term neonate at 10 minutes postdelivery Which of the following respiratory function variables considerably differ (mL/kg or mL/kg/min) between infant and grownup Oxygen consumption 34 Anesthesia for Thoracic Surgery Katherine Marseu Peter Slinger the most common indication for thoracic surgery is malignancy (1,2,3). Despite this, a broad variety of pathologies and procedures are commonly encountered when providing anesthetics for sufferers undergoing thoracic surgery. As a result, there are a variety of essential preoperative, intraoperative, and postoperative anesthetic concerns for thoracic surgery. Preoperative Assessment Respiratory and cardiac problems are the major cause of perioperative morbidity and mortality within the thoracic surgical population. Thus, the preoperative evaluation of those patients focuses on an assessment of respiratory perform and the cardiopulmonary interplay. All pulmonary resection sufferers should have preoperative spirometry to decide postoperative preservation of respiratory perform, which has been shown to be proportional to the remaining number of lung subsegments (right upper, center, and lower lobes = 6,4,12 subsegments, respectively; left higher and decrease lobes = 10 subsegments each, for a total of 42 subsegments). Cardiopulmonary Interaction the most important evaluation of respiratory operate is an assessment of the cardiopulmonary reserve, and the maximal oxygen consumption. Common Pathologies and Comorbidities Malignancies the overwhelming majority of sufferers presenting for thoracic surgical procedure will have a malignancy, together with lung cancers, pleural and mediastinal tumors, and esophageal most cancers. Chronic Obstructive Pulmonary Disease this is the commonest concurrent illness within the thoracic surgical inhabitants. Patients ought to be free of exacerbation before elective surgical procedure, and will have fewer postoperative pulmonary issues when intensive chest physiotherapy is initiated preoperatively. Pulmonary complications are additionally decreased in thoracic surgical patients who stop smoking for more than four weeks before surgery. Other issues in continual obstructive pulmonary disease sufferers embrace the presence of bullous illness, pulmonary hypertension with right coronary heart dysfunction, and the risk of dynamic hyperinflation because of fuel trapping (1,2,3). A central venous line may be required in some circumstances for vascular access or for infusion of vasoactive drugs. Fluid administration for all thoracic procedures should comply with both a restricted or a goal-directed protocol. However, recently, issues about acute kidney injury have called into question the strategy of fluid restriction in thoracic surgery (3). Physiology of One-Lung Ventilation In the overwhelming majority of thoracic surgical procedure cases, sufferers transition from being upright, awake, and spontaneously respiratory to supine, asleep, and paralyzed. This change will be magnified by the induction of anesthesia and administration of muscle relaxants. When upright, the majority of ventilation and perfusion reach the gravity-dependent parts of the lungs. Second, in the lateral place, the dependent lung receives more perfusion compared with the nondependent lung. Third, when the chest is opened, the compliance of the nondependent lung improves relative to the. The highest priorities embody prevention of contamination of the healthy lung by an infection Fractional blood circulate 40% PaO2 = 400 mm Hg � � Qs/Qt = 10% 60% Dependent lung Two-lung ventilation vs. Typical values for fractional blood circulate to the nondependent and de� � pendent lungs, as nicely as PaO2 and Q s/Q t for the two conditions, are proven. The � � Q s/Q t during two-lung air flow is assumed to be distributed equally between the two lungs (5% to each lung). The 35% of whole circulate perfusing the nondependent lung, which was not shunt move, was assumed to be succesful of cut back its blood move by 50% by hypoxic pulmonary vasocon� � striction. Several advantages of the blocker include the flexibleness for use in an oral or nasotracheal fashion and for selective lobar blockade. It is particularly useful in scenarios similar to a difficult airway or the need for postoperative air flow. When properly positioned (right), the distal "bronchial lumen" is placed within the left mainstem bronchus proximal to the left higher lobe orifice, with the "bronchial cuff" inflated simply distal to the carina within the left mainstem bronchus. The proximal "tracheal lumen" is positioned above the carina, with the "tracheal cuff" inflated within the mid-trachea. Proper positioning allows for the choices of one-lung air flow on either side (with contralateral lung deflation), as properly as two-lung air flow. This is very detrimental in a situation where lack of lung separation can result in contamination from blood or pus (1,3). Whether utilizing volume-controlled or pressure-controlled air flow, tidal quantity should be roughly 5 mL/kg. Peak airway pressures must be maintained at <35 cm H2O, and ideally <25 cm H2O (1,3). In the presence of bullous disease, even lower airway pressures must be thought-about. Management of Hypoxemia on One-Lung Ventilation Hypoxic pulmonary vasoconstriction can take hours to attain full effect. Bronchoscopic view of the carina via the distal opening of a normal endotracheal tube. Note the C-shaped tracheal rings anteriorly orient the viewer to the left and proper mainstem bronchi.
Diabecon 60 caps order without prescription
There are two: the greater omentum derived from the dorsal mesentery metabolic disease associates inc diabecon 60 caps buy on line, and the lesser omentum derived from the ventral mesentery diabetes signs symptoms type 2 60 caps diabecon order with visa. Greater omentum the larger omentum is a large, apron-like, peritoneal fold that attaches to the greater curvature of the stomach and the rst part of the duodenum. It drapes inferiorly over the transverse colon and the coils of the jejunum and ileum. Turning posteriorly, it ascends to associate with, and turn out to be adherent to , the peritoneum on the superior surface of the transverse colon and the anterior layer of the transverse mesocolon before arriving on the posterior stomach wall. Usually a thin membrane, the greater omentum at all times contains an accumulation of fats, which may become substantial in some people. Additionally, there are two Clinical app Peritoneal unfold of illness the large floor space of the peritoneal cavity allows an infection and malignant illness to unfold simply all through the stomach. This peritoneal gas can be easily visualized on a chest radiograph, with the patient standing, the place gas can be demonstrated in extremely small amounts beneath the diaphragm. Regional anatomy � Abdominal viscera arteries and accompanying veins, the right and left gastro-omental vessels, between this double-layered peritoneal apron just inferior to the higher curvature of the abdomen. Les s er omentum Hepatogas tric ligament Hepatoduodenal Liver (retracted) Les s er ligament curvature of the s tomach Gallbladder Omental foramen Duodenum Stomach four Lesser omentum the opposite two-layered peritoneal omentum is the lesser omentum. It extends from the lesser curvature of the stomach and the rst part of the duodenum to the inferior surface of the liver. A skinny membrane continuous with the peritoneal coverings of the anterior and posterior surfaces of the stomach and the rst part of the duodenum, the lesser omentum is divided into: a medial hepatogastric ligament, which passes between the stomach and liver, and a lateral hepatoduodenal ligament, which passes between the duodenum and liver. The hepatoduodenal ligament ends laterally as a free margin and serves as the anterior border of the omental foramen. Enclosed on this free edge are the hepatic artery correct, the bile duct, and the portal vein. Additionally, the proper and left gastric vessels are between the layers of the lesser omentum close to the lesser curvature of the abdomen. Clinical app the greater omentum When a laparotomy is carried out and the peritoneal cavity is opened, the rst structure often encountered is the greater omentum. This fatty double-layered vascular membrane hangs like an apron from the greater curvature of the abdomen, drapes over the transverse colon, and lies freely suspended inside the abdominal cavity. It is commonly referred to because the "policeman of the abdomen" due to its apparent capability to migrate to any in amed area and wrap itself around the organ to wall off in ammation. Direct omental spread by a transcoelomic route is frequent for carcinoma of the ovary. Mesentery the mesentery is a big, fan-shaped, double-layered fold of peritoneum that connects the jejunum and ileum to the posterior belly wall. Its superior attachment is on the duodenojejunal junction, simply to the left of the upper lumbar a half of the vertebral column. It passes obliquely downward and to the best, ending at the ileocecal junction near the higher border of the right sacro-iliac joint. In the fats between the 2 peritoneal layers of the mesentery are the arteries, veins, nerves, and lymphatics that offer the jejunum and ileum. Transverse mesocolon the transverse mesocolon is a fold of peritoneum that connects the transverse colon to the posterior stomach wall. Its two layers of peritoneum leave the posterior belly wall throughout the anterior floor of the top and physique of the pancreas and pass outward to surround the transverse colon. Between its layers are the arteries, veins, nerves, and lymphatics related to the transverse colon. The anterior layer of the transverse mesocolon is adherent to the posterior layer of the larger omentum. Sigmoid mesocolon the sigmoid mesocolon is an inverted, V-shaped peritoneal fold that attaches the sigmoid colon to the stomach wall. The apex of the V is near the division of the left frequent iliac artery into its inner and exterior branches, with the left limb of the descending V alongside the medial border of the left psoas major muscle and the right Mesenteries Mesenteries are peritoneal folds that connect viscera to the posterior abdominal wall. They permit some motion and supply a conduit for vessels, nerves, and lymphatics to attain the viscera and include: the mesentery-associated with components of the small gut, the transverse mesocolon-associated with the transverse colon, and the sigmoid mesocolon-associated with the sigmoid colon. The sigmoid and superior rectal vessels, together with the nerves and lymphatics related to the sigmoid colon, pass by way of this peritoneal fold. Ligaments Similarly, the posterior vagal trunk consists of a single trunk whose bers largely come from the right vagus nerve, and rotational modifications during development move this trunk to the posterior floor of the esophagus. [newline]Peritoneal ligaments encompass two layers of peritoneum that join two organs to one another or connect an organ to the physique wall, and should form a half of an omentum. For instance, the splenorenal ligament connects the left kidney to the spleen and the gastrophrenic ligament connects the abdomen to the diaphragm. Stomach the abdomen is essentially the most dilated part of the gastrointestinal tract and has a J-like form. Positioned between the stomach esophagus and the small gut, the abdomen is in the epigastric, umbilical, and left hypochondrium regions of the abdomen. Organs Abdominal esophagus the stomach esophagus represents the short distal part of the esophagus situated within the abdominal cavity. Associated with the esophagus, because it enters the abdominal cavity, are the anterior and posterior vagal trunks: the anterior vagal trunk consists of several smaller trunks whose bers largely come from the left vagus nerve; rotation of the gut during improvement moves these trunks to the anterior floor of the esophagus; 154 Regional anatomy � Abdominal viscera Short fuel tric arteries Splenic artery Left fuel tric artery Right gasoline tric artery Hepatic artery proper four Abdominal es ophagus Cardial notch Fundus Cardia Les s er curvature Angular incis ure Pyloric orifice Left fuel troomental artery Right gasoline tro-omental artery Abdominal aorta Duodenum Pyloric canal Pyloric s phincter Pyloric cons triction Body Pyloric antrum Greater curvature. Pos terior s uperior pancreaticoduodenal artery Anterior s uperior pancreaticoduodenal artery Gas troduodenal artery. Imaging app the most distal portion of the pyloric part of the abdomen is the pylorus. It is marked on the floor of the organ by the pyloric constriction and contains a thickened ring of gastric round muscle, the pyloric sphincter, which surrounds the distal opening of the abdomen, the pyloric ori ce. Other options of the stomach embody: the greater curvature, which is some extent of attachment for the gastrosplenic ligament and the greater omentum; the lesser curvature, which is some extent of attachment for the lesser omentum; the cardial notch, which is the superior angle created when the esophagus enters the abdomen; and the angular incisure, which is a bend on the lesser curvature. Visualizing the abdomen Superior part of duodenum Es ophagus Pyloric antrum Fundus of s tomach the arterial supply to the abdomen. This hole tube, which is approximately 6 to 7 m long with a narrowing diameter from starting to finish, consists of the duodenum, the jejunum, and the ileum. This C-shaped construction, adjacent to the head of the pancreas, is 20 to 25 cm long and is above the level of the umbilicus; its lumen is the widest of the small intestine. It is retroperitoneal aside from its beginning, which is related to the liver by the hepatoduodenal ligament, a half of the lesser omentum. Clinically, the beginning of this a part of the duodenum is referred to as the ampulla or duodenal cap, and most duodenal ulcers occur on this part of the duodenum. This part of the duodenum contains the main duodenal papilla, which is the common entrance for the bile and pancreatic ducts, and the minor duodenal papilla, which is the entrance for the accent pancreatic duct, and the junction of the foregut and the midgut just under the main duodenal papilla. The inferior part (third part) of the duodenum is the longest section, crossing the inferior vena cava, the aorta, and the vertebral column. This duodenojejunal exure is surrounded by a fold of peritoneum containing muscle bers referred to as the suspensory muscle (ligament) of duodenum (ligament of Treitz). Regional anatomy � Abdominal viscera Pos terior s uperior pancreaticoduodenal artery Hepatic artery correct Gas troduodenal artery Supraduodenal artery Right gasoline troomental artery 4 Left gasoline tric artery Imaging app Visualizing the jejunum and ileum J ejunum Anterior s uperior pancreaticoduodenal artery Pos terior inferior pancreaticoduodenal artery Superior mes enteric artery Abdominal aorta Anterior inferior pancreaticoduodenal artery. The arterial supply to the jejunum contains jejunal arteries from the superior mesenteric artery. Ileum Jejunum the jejunum and ileum make up the last two sections of the small intestine. It is usually within the left higher quadrant of the abdomen and is bigger in diameter and has a thicker wall than the ileum.

Diabecon 60 caps discount amex
T12 L1 Iliohypogas tric nerve Ilio-inguinal nerve Genitofemoral nerve L3 Lateral cutaneous nerve of thigh L4 To iliacus mus cle Femoral nerve Obturator nerve To lumbos acral trunk L2 Iliohypogastric and ilio-inguinal nerves (L1) the iliohypogastric and ilio-inguinal nerves arise as a single trunk from the anterior ramus of nerve L1 diabetes life expectancy diabecon 60 caps buy discount. Either before or soon after emerging from the lateral border of the psoas main muscle diabetic jelly recipes discount diabecon 60 caps amex, this single trunk divides into the iliohypogastric and the ilio-inguinal nerves. It pierces the transversus abdominis muscle and continues anteriorly around the physique between the transversus abdominis and inner oblique muscular tissues. Above the iliac crest, a lateral cutaneous department pierces the internal and exterior indirect muscle tissue to provide the posterolateral gluteal skin. The remaining a half of the iliohypogastric nerve (the anterior cutaneous branch) continues in an anterior course, piercing the internal oblique simply medial to the anterior superior iliac backbone because it continues in an obliquely downward and medial direction. Becoming cutaneous, just above the tremendous cial inguinal ring, after piercing the aponeurosis of the external oblique, it distributes to the pores and skin within the pubic area. Ilio-inguinal nerve the ilio-inguinal nerve is smaller than, and inferior to , the iliohypogastric nerve because it crosses the quadratus lumborum muscle. Its course is extra oblique than that of the iliohypogastric nerve, and it often crosses part of the iliacus muscle on its approach to the iliac crest. Near the anterior end of the iliac crest, it pierces the transversus abdominis muscle, and then pierces the internal indirect muscle and enters the inguinal canal. The ilio-inguinal nerve emerges via the tremendous cial inguinal ring, along with the spermatic twine, and provides cutaneous innervation to the upper medial thigh, the foundation of the penis, and the anterior floor of the scrotum in males, or the mons pubis and labium majus in ladies. Genitofemoral nerve (L1 and L2) the genitofemoral nerve arises from the anterior rami of the nerves L1 and L2. It passes downward in the substance of the psoas main muscle till it emerges on the anterior surface of psoas major. It then descends on the floor of the muscle, in a retroperitoneal place, Subcos tal nerve Iliohypogas tric nerve Ilio-inguinal nerve Lateral cutaneous nerve of thigh Subcos tal nerve (T12) Ps oas main mus cle Iliohypogas tric nerve (L1) Ilio-inguinal nerve (L1) Genitofemoral nerve (L1,L2) Iliacus mus cle Femoral nerve Genitofemoral nerve Obturator nerve Lateral cutaneous nerve of thigh (L2,L3) Femoral nerve (L2 to L4) Obturator nerve (L2 to L4) Lumbos acral trunks (L4,L5) 204. Regional anatomy � Posterior stomach region T10 T11 T12 Lateral cutaneous department of iliohypogas tric nerve (L1) Anterior cutaneous department of iliohypogas tric nerve (L1) Ilio-inguinal nerve (L1) Femoral branch of genitofemoral nerve (L1,L2) Lateral cutaneous nerve of thigh (L2,L3) Cutaneous department of obturator nerve (L2 to L4) Intermediate cutaneous from femoral nerve Femoral nerve (L2 to L4) Medial cutaneous from femoral nerve four T10 T11 T12 Genitofemoral nerve (L1,L2) Ilio-inguinal nerve (L1) Lateral cutaneous nerve of thigh (L2,L3) Obturator nerve (L2 to L4) T12 L1 Saphenous nerve from femoral nerve. The genital department continues downward and enters the inguinal canal via the deep inguinal ring. It continues via the canal and: In males, innervates the cremasteric muscle and terminates on the pores and skin in the higher anterior part of the scrotum; and In women, accompanies the spherical ligament of the uterus and terminates on the skin of the mons pubis and labium majus. The femoral department descends on the lateral facet of the external iliac artery and passes posterior to the inguinal ligament, getting into the femoral sheath lateral to the femoral artery. It pierces the anterior layer of the femoral sheath and the fascia lata to provide the skin of the upper anterior thigh. The lateral cutaneous nerve of thigh supplies the skin on the anterior and lateral thigh to the extent of the knee. Obturator nerve (L2 to L4) Lateral cutaneous nerve of thigh (L2 and L3) the lateral cutaneous nerve of thigh arises from the anterior rami of nerves L2 and L3. It emerges from the lateral border of the psoas main muscle, passing obliquely downward across the iliacus muscle toward the anterior superior iliac spine. It descends in the psoas main muscle, emerging from its medial facet close to the pelvic brim. The obturator nerve continues posterior to the frequent iliac vessels, passes throughout the lateral wall of the pelvic cavity, and enters the obturator canal, through which the obturator nerve features entry to the medial compartment of the thigh. In the realm of the obturator canal, the obturator nerve divides into anterior and posterior branches. On entering the medial compartment of the thigh, the two branches are separated by the obturator externus and adductor brevis muscle tissue. Throughout their course by way of the medial compartment, these two branches provide: articular branches to the hip joint, muscular branches to obturator externus, pectineus, adductor longus, gracilis, adductor brevis, and adductor magnus muscles, cutaneous branches to the medial aspect of the thigh, and 205 Abdomen in affiliation with the saphenous nerve, cutaneous branches to the medial side of the upper part of the leg, and articular branches to the knee joint. Femoral nerve (L2 to L4) the femoral nerve arises from the anterior rami of nerves L2 to L4. It descends via the substance of the psoas main muscle, emerging from the lower lateral border of the psoas main. Continuing its descent, the femoral nerve lies between the lateral border of the psoas main and the anterior surface of the iliacus muscle. It is deep to the iliacus fascia and lateral to the femoral artery because it passes posterior to the inguinal ligament and enters the anterior compartment of the thigh. Muscular branches innervate the iliacus, pectineus, sartorius, rectus femoris, vastus medialis, vastus intermedius, and vastus lateralis muscular tissues. The true pelvis (lesser pelvis) is related to the inferior components of the pelvic bones, sacrum, and coccyx, and has an inlet and an outlet. This cavity is steady superiorly with the stomach cavity and contains and supports elements of the urinary, gastrointestinal, and reproductive techniques. The perineum contains and supports the external genitalia and exterior openings of the genitourinary and gastrointestinal methods. Pelvic bone the pelvic bone is irregular in shape and has two main elements separated by an indirect line on the medial surface of the bone. The pelvic bone under this line represents the lateral wall of the true pelvis, which incorporates the pelvic cavity. The linea terminalis is the decrease two-thirds of this line and contributes to the margin of the pelvic inlet. The lateral floor of the pelvic bone has a large articular socket, the acetabulum, which along with the pinnacle of the femur, types the hip joint. Inferior to the acetabulum is the massive obturator foramen, most of which is closed by a at connective tissue membrane, the obturator membrane. A small obturator canal stays open superiorly between the membrane and adjoining bone, offering a route of communication between the lower limb and the pelvic cavity. The posterior margin of the bone is marked by two notches separated by the ischial spine. Regional anatomy � Pelvis 5 the larger sciatic notch, and the lesser sciatic notch. The irregular anterior margin of the pelvic bone is marked by the anterior superior iliac spine, the anterior inferior iliac spine, and the pubic tubercle. Components of the pelvic bone Each pelvic bone is fashioned by three elements: the ilium, pubis, and ischium. At birth, these bones are related by cartilage within the area of the acetabulum; later, Ilium Of the three elements of the pelvic bone, the ilium is essentially the most superior in place. The ilium is separated into upper and decrease parts by a ridge on the medial surface. Posteriorly, the ridge is sharp and lies immediately superior to the floor of the bone that articulates with the sacrum. This sacral surface has a large L-shaped facet for articulating with the sacrum and an expanded, posterior roughened space for the attachment of the strong ligaments that assist the sacro-iliac joint. Anteriorly, the ridge separating the upper and decrease components of the ilium is rounded and termed the arcuate line. The portion of the ilium mendacity inferiorly to the arcuate line is the pelvic part of the ilium and contributes to the wall of the lesser or true pelvis. The upper part of the ilium expands to kind a at, fanshaped "wing," which supplies bony support for the lower abdomen, or false pelvis.
Diseases
- Aldolase A deficiency
- Factor II deficiency
- Aberrant subclavian artery
- Billard Toutain Maheut syndrome
- Pulmonary alveolar proteinosis, congenital
- Creutzfeldt Jakob disease
- Proteus syndrome
- Craniosynostosis Maroteaux Fonfria type
- Hersh Podruch Weisskopk syndrome
Discount diabecon 60 caps amex
Superiorly is the diaphragm and inferior to this prediabetes definition hba1c buy cheap diabecon 60 caps line, moving in a medial to lateral direction diabetes treatment options diabecon 60 caps order with visa, are psoas main, quadratus lumborum, and transversus abdominis muscular tissues. The pleural sacs, and speci cally, the costodiaphragmatic recesses, subsequently lengthen posterior to the kidneys. Also passing posterior to the kidneys are the subcostal vessels and nerves and the iliohypogastric and ilio-inguinal nerves. Renal fats and fascia the kidneys are enclosed in and related to a novel arrangement of fascia and fats. The suprarenal glands are additionally enclosed on this fascial compartment, normally separated from the kidneys by a skinny septum. At the lateral margins of each kidney, the anterior and posterior layers of the renal fascia fuse. This fused layer could connect with the transversalis fascia on the lateral abdominal wall. Above each suprarenal gland, the anterior and posterior layers of the renal fascia fuse and mix with the fascia that covers the diaphragm. Pyramid in renal medulla Renal column Renal cortex Renal papilla Major calyx Renal artery Hilum of kidney In addition to perinephric fats and the renal fascia, a nal layer of paranephric fat (pararenal fat) completes the fats and fascias associated with the kidney. In some cases, the anterior layer might cross the midline to the alternative facet and mix with its companion layer. The posterior layer of the renal fascia passes medially between the kidney and the fascia covering the quadratus lumborum muscle to fuse with the fascia covering the psoas major muscle. Inferiorly, the anterior and posterior layers of the renal fascia enclose the ureters. Each kidney has a easy anterior and posterior floor covered by a brous capsule, which is easily detachable besides throughout illness. On the medial margin of each kidney is the hilum of kidney, which is a deep vertical slit through which renal vessels, lymphatics, and nerves enter and go away the substance of the kidney. The renal cortex is a steady band of pale tissue that fully surrounds the renal medulla. Extensions of the renal cortex (the renal columns) project into the inside aspect of the kidney, dividing the renal medulla into discontinuous aggregations of triangular-shaped tissue (the renal pyramids). The bases of the renal pyramids are directed outward, towards the renal cortex, whereas the apex of every renal pyramid initiatives inward, towards the renal sinus. The apical projection (renal papilla) contains the openings of the papillary ducts draining the renal tubules and is surrounded by a minor calyx. The minor calices obtain urine from the papillary ducts and characterize the proximal parts of the tube that may finally kind the ureter. In the renal sinus, several minor calices unite to kind a significant calyx, and two or three major calices unite to type the renal pelvis, which is the funnel-shaped superior end of the ureters. Regional anatomy � Posterior belly area iliac or the start of the exterior iliac arteries, enter the pelvic cavity, and proceed their journey to the bladder. Renal vasculature and lymphatics A single large renal artery, a lateral department of the stomach aorta, provides every kidney. The left renal artery often arises somewhat larger than the right, and the right renal artery is longer and passes posterior to the inferior vena cava. As every renal artery approaches the renal hilum, it divides into anterior and posterior branches, which supply the renal parenchyma. They originate from the lateral side of the stomach aorta, either above or beneath the first renal arteries, enter the hilum with the primary arteries or move directly into the kidney at another stage, and are generally known as extrahilar arteries. Multiple renal veins contribute to the formation of the left and proper renal veins, both of that are anterior to the renal arteries. Importantly, the longer left renal vein crosses the midline anterior to the abdominal aorta and posterior to the superior mesenteric artery and could be compressed by an aneurysm in both of these two vessels. The lymphatic drainage of each kidney is to the lateral aortic (lumbar) nodes across the origin of the renal artery. The ureters obtain arterial branches from adjoining vessels as they move toward the bladder. The center part could obtain branches from the stomach aorta, the testicular or ovarian arteries, and the frequent iliac arteries. In the pelvic cavity, the ureters are equipped by one or more arteries from branches of the inner iliac arteries. In all instances, arteries reaching the ureters divide into ascending and descending branches, which form longitudinal anastomoses. Lymphatic drainage of the ureters follows a pattern much like that of the arterial supply. They are continuous superiorly with the renal pelvis, which is a funnel-shaped structure within the renal sinus. The renal pelvis is formed from a condensation of two or three main calices, which in flip are formed by the condensation of several minor calices. The renal pelvis narrows as it passes inferiorly by way of the hilum of the kidney and becomes steady with the ureter on the ureteropelvic junction. Inferior to this junction, the ureters descend retroperitoneally on the medial aspect of the psoas major muscle. At the pelvic brim, the ureters cross both the top of the common External iliac artery. The inferior a half of each ureter drains to lymph nodes associated with the exterior and internal iliac vessels. Clinical app Kidney transplant Kidney transplantation began in the United States within the Fifties. Since the rst transplant, the main problem for kidney transplantation has been tissue rejection. A number of years have passed since this initial procedure and there have been signi cant breakthroughs in transplant rejection medicine. Renal transplantation is now a common process undertaken in patients with end-stage renal failure. An best place to situate the transplant kidney is within the left or the right iliac fossa. The exterior indirect muscle, inner oblique muscle, transverse abdominis muscle, and transversalis fascia are divided. The parietal peritoneum is medially retracted to reveal the external iliac artery, exterior iliac vein, and the bladder. In some situations the interior iliac artery of the recipient is mobilized and anastomosed directly as an end-to-end procedure onto the renal artery of the donor kidney. The ureter is definitely tunneled obliquely via the bladder wall with a straightforward anastomosis.
Diabecon 60 caps visa
Parietal pleura Vis ceral pleura Clinical app the association of pleural cavities is clinically signi cant the pleural cavities are completely separated from each other by the mediastinum blood glucose 246 60 caps diabecon with amex. This also signifies that the mediastinum can be entered surgically with out opening the pleural cavities diabetes in dogs and panting diabecon 60 caps on-line. Another essential function of the pleural cavities is that they lengthen above the level of rib I. As a consequence, abnormal events within the root of the neck can contain the adjacent pleura and lung, and occasions in the adjoining pleura and lung can contain the basis of the neck. Medias tinum Left pleural cavity Cos todiap hragmatic reces s Diaphragm Right pleural cavity 78. This sleevelike overlaying, and the structures it accommodates, types the basis of the lung. The root joins the medial surface of the lung at an area referred to because the hilum of lung. The costal pleura is innervated by branches from the intercostal nerves and pain can be felt in relation to the thoracic wall. The diaphragmatic pleura and the mediastinal pleura are innervated primarily by the phrenic nerves (originating at spinal cord ranges C3, C4, and C5). Pain from these areas would discuss with the C3, C4, and C5 dermatomes (lateral neck and the supraclavicular area of the shoulder). The visceral pleural is innervated by visceral afferent bers that accompany bronchial vessels and pain is generally not elicited from this tissue. Each pleural cavity is the potential area enclosed between the visceral and parietal pleurae. As a end result, the floor of the lung, which is roofed by visceral pleura, directly opposes and freely slides over the parietal pleura attached to the wall. The peripheral re ections of parietal pleura mark the extent of the pleural cavities. The dome-shaped layer of parietal pleura lining the cervical extension of the pleural cavity is cervical pleura (dome of pleura or pleural cupola). Covering the superior surface of the cervical pleura is a distinct domelike layer of fascia, the suprapleural membrane. Superiorly, the membrane receives muscle bers from a few of the deep muscular tissues within the neck (scalene muscles) that function to maintain the membrane taught. The suprapleural membrane offers apical support for the pleural cavity within the root of the neck. This limitation is brought on by the inferior slope of rib I to its articulation with the manubrium. Anteriorly, the pleural cavities strategy one another posterior to the upper a half of the sternum. The largest and clinically most essential recesses are the costodiaphragmatic recesses, which occur in each pleural cavity between the costal pleura and diaphragmatic pleura. The costodiaphragmatic recesses are the regions between the inferior margin of the lungs and inferior margin of the pleural cavities. During expiration, the inferior margin of the lung rises and the costodiaphragmatic recess turns into bigger. Costodiaphragmatic recesses Visceral pleura the visceral pleura is continuous with the parietal pleura at the hilum of every lung where structures enter and go away the organ. The visceral pleura is rmly attached to the floor of the lung, including both opposed surfaces of the ssures that divide the lungs into lobes. Expansion of the lungs into these spaces usually occurs only during compelled inspiration; the recesses additionally provide potential spaces during which uids can gather and from which uids could be aspirated. Costomediastinal recesses Anteriorly, a costomediastinal recess happens on both sides where the costal pleura is against the mediastinal pleura. As the uid accumulates throughout the pleural area the underlying lung is compromised and should collapse as the quantity of uid increases. Once a pleural effusion has been recognized, uid usually will be aspirated to decide the trigger, which may embrace infection, malignancy, cardiac failure, hepatic disease, and pulmonary embolism. Lungs the two lungs are organs of respiration and lie on both side of the mediastinum surrounded by the proper and left pleural cavities. Air enters and leaves the lungs via the primary bronchi, which are branches of the trachea. The pulmonary arteries deliver deoxygenated blood to the lungs from the best ventricle of the center. The right lung is normally slightly bigger than the left lung as a result of the middle mediastinum, containing the center, bulges more to the left than to the proper. Each lung has a half-cone form, with a base, apex, two surfaces, and three borders. The two surfaces-the costal floor lies instantly adjacent to the ribs and intercostal areas of the thoracic wall. The mediastinal floor lies in opposition to the mediastinum anteriorly and the vertebral column posteriorly and accommodates the comma-shaped hilum of the lung through which constructions enter and leave. The three borders-the inferior border of the lung is sharp and separates the bottom from the costal surface. The anterior and posterior borders separate the costal surface from the medial surface. Unlike the anterior and inferior borders, which are sharp, the posterior border is clean and rounded. The lungs lie directly adjoining to , and are indented by, buildings contained in the overlying space. The heart and main vessels kind bulges in the mediastinum that indent the medial surfaces of the lung; the ribs indent the costal Clinical app Pneumothorax A pneumothorax is a collection of fuel or air inside the pleural cavity. When air enters the pleural cavity the tissue elasticity of the parenchyma causes the lung to collapse within the chest impairing lung perform. Occasionally, the gasoline throughout the pleural cavity might accumulate to such an extent that the mediastinum is "pushed" to the opposite aspect, compromising the opposite lung. The symptoms of pneumothorax are often determined by the degree of air leak and the rate at which the buildup of gasoline occurs and the following lung collapse. Right lung Apex Anterior border Left lung Hilum Bronchus Pulmonary artery Pulmonary veins Pos terior border Cos tal s urface Medias tinal s urface Inferior border Bas e (diaphragmatic s urface). Pathology, such as tumors, or abnormalities in one construction can have an effect on the associated structure. Root and hilum the root of every lung is a brief tubular assortment of structures that together connect the lung to structures in the mediastinum. It is roofed by a sleeve of mediastinal pleura that re ects onto the surface of the lung as visceral pleura. The region outlined by this pleural re ection on the medial floor of the lung is the hilum, where buildings enter and leave. A thin blade-like fold of pleura tasks inferiorly from the basis of the lung and extends from the hilum to the mediastinum. It may stabilize the position of the inferior lobe and may accommodate the down-and-up translocation of buildings within the root during respiratory. In the mediastinum, the vagus nerves cross immediately posterior to the roots of the lungs, whereas the phrenic nerves cross immediately anterior to them.
Best 60 caps diabecon
Regional anatomy � Perineum Anteriorly blood sugar safe zone diabecon 60 caps buy online, in the urogenital triangle diabetes mellitus type 2 ayurvedic treatment buy diabecon 60 caps otc, a U-shaped defect in the muscle tissue, the urogenital hiatus, allows the passage of the urethra and vagina. This is best accomplished with sufferers mendacity on their backs with their thighs exed and kidnapped in the lithotomy position. The ischial tuberosities are palpable on all sides as massive bony lots near the crease of skin (gluteal fold) between the thigh and gluteal region. The tip of the coccyx is palpable within the midline posterior to the anal aperture and marks the most posterior limit of the perineum. In males, the pubic symphysis is palpable instantly superior to the place the physique of the penis joins the decrease belly wall. Imaginary strains that be a part of the ischial tuberosities with the pubic symphysis in front, and with the tip of the coccyx behind, define the diamond-shaped perineum. An additional line between the ischial tuberosities divides the perineum into two triangles, the urogenital triangle anteriorly and anal triangle posteriorly. This line also approximates the position of the posterior margin of the perineal membrane. The midpoint of this line marks the location of the perineal body or central tendon of the perineum. It has a free posterior border, which is anchored within the midline to the perineal body and is attached laterally to the pubic arch. Immediately superior to the perineal membrane is a skinny region termed the deep perineal pouch, containing a layer of skeletal muscle and neurovascular tissues. The perineal membrane and deep perineal pouch present help for the exterior genitalia, that are hooked up to its inferior surface. Also, the parts of the perineal membrane and deep perineal pouch inferior to the urogenital hiatus within the levator ani present help for pelvic viscera. The urethra leaves the pelvic cavity and enters the perineum by passing by way of the deep perineal pouch and perineal membrane. In ladies, the vagina also passes through these constructions posterior to the urethra. In the anal triangle, these gutters, one on each side of the anal aperture, are termed ischio-anal fossae. The medial and lateral partitions converge superiorly the place the levator ani muscle attaches to the fascia overlying the obturator internus muscle. The ischio-anal fossae enable motion of the pelvic diaphragm and expansion of the anal canal throughout defecation. The ischio-anal fossae of the anal triangle are steady anteriorly with recesses that project into the urogenital triangle superior to the deep perineal pouch. Clinical app Abscesses in the ischio-anal fossae the anal mucosa is particularly weak to injury and may be simply torn by hard feces. Occasionally, sufferers develop in ammation and infection of the anal canal (sinuses or crypts), which can unfold laterally into the ischio-anal fossae or superiorly into the pelvic cavity. The ceiling of the anal triangle is the pelvic diaphragm, which is formed by the levator ani and coccygeus muscles. The anal aperture happens centrally in the anal triangle and is said on both side to an ischio-anal fossa. The exterior anal sphincter, which surrounds the anal canal, is shaped by skeletal muscle and consists of three parts-deep, super cial, and subcutaneous- organized sequentially alongside the canal from superior to inferior (Table 5. The external anal sphincter is innervated by inferior rectal branches of the pudendal nerve and by branches directly from the anterior ramus of S4. Bulbourethral gland within d eep pouch Urogenital triangle the urogenital triangle of the perineum is the anterior half of the perineum and is oriented within the horizontal airplane. Surrounds decrease a part of anal canal Horizontally attened disc that surrounds the anal aperture simply beneath the skin. Anchored anteriorly to the perineal body and posteriorly to the anococcygeal body Pudendal nerve (S2 and S3) and branches instantly from S4 Muscles of pelvic wall External anal sphincter Deep half Super cial half Subcutaneous half 246 Regional anatomy � Perineum As with the anal triangle, the roof or ceiling of the urogenital triangle is the levator ani muscle. Unlike the anal triangle, the urogenital triangle accommodates a robust bromuscular support platform, the perineal membrane, and deep perineal pouch (see p. Anterior extensions of the ischio-anal fossae happen between the deep perineal pouch and the levator ani muscle on both sides. Between the perineal membrane and the membranous layer of tremendous cial fascia is the tremendous cial perineal pouch. The principal constructions in this pouch are the erectile tissues of the penis and clitoris and related skeletal muscular tissues. Unlike the root of penis, the basis of clitoris technically consists only of the two crura. The body of clitoris is supported by a suspensory ligament that attaches superiorly to the pubic symphysis. The glans clitoris is connected to the distal end of the physique and is connected to the bulbs of the vestibule by small bands of erectile tissue. The glans clitoris is exposed within the perineum and the physique of the clitoris can be palpated via skin. Structures within the super cial perineal pouch the tremendous cial perineal pouch incorporates. Each erectile construction consists of a central core of expandable vascular tissue and its surrounding connective tissue capsule. Erectile tissues Two units of erectile buildings be part of to kind the penis and the clitoris. A pair of cylindrically formed corpora cavernosa, one on all sides of the urogenital triangle, are anchored by their proximal ends to the pubic arch. These hooked up parts are sometimes termed the crura (from the Latin for "legs") of the clitoris or the penis. The second set of erectile tissues surrounds the openings of the urogenital system. In women, a pair of erectile buildings, termed the bulbs of vestibule, are located one on all sides on the vaginal opening and are rmly anchored to the perineal membrane. Small bands of erectile tissues connect the anterior ends of those bulbs to a single, small, pea-shaped erectile mass, the glans clitoris, which is positioned within the midline on the finish of the physique of the clitoris and anterior to the opening of the urethra. In men, a single massive erectile mass, the corpus spongiosum, is the structural equal to the bulbs of the vestibule, the glans clitoris, and the interconnecting bands of erectile tissues in women. The corpus spongiosum is anchored at its base (bulb of penis) to the perineal membrane. In men, the urethra is enclosed by the corpus spongiosum and opens at the end of the penis. Penis the penis consists mainly of the two corpora cavernosa and the only corpus spongiosum, which accommodates the urethra. The body of penis, which is covered entirely by pores and skin, is formed by the tethering of the 2 proximal free components of the corpora cavernosa and the related free a part of the corpus spongiosum. The base of the body of penis is supported by two ligaments: the suspensory ligament of penis (attached superiorly to the pubic symphysis), and the more tremendous cially positioned fundiform ligament of penis (attached above to the linea alba of the anterior abdominal wall and splits under into two bands that move on both sides of the penis and unite inferiorly). Because the anatomical position of the penis is erect, the paired corpora are de ned as dorsal in the body of the penis and the single corpus spongiosum as ventral, despite the precise fact that the positions are reversed within the nonerect (accid) penis.
Cheap diabecon 60 caps free shipping
On the other hand diabetes medications pen discount diabecon 60 caps mastercard, the periosteum is equipped with numerous sensory nerve bers and is very sensitive to any kind of harm blood sugar 108 discount 60 caps diabecon overnight delivery. Developmentally, all bones come from mesenchyme by both intramembranous ossi cation, by which mesenchymal fashions of bones bear ossi cation, or endochondral ossi cation, by which cartilaginous fashions of bones form from mesenchyme and endure ossi cation. Clinical app Bone marrow transplants There are two forms of bone marrow, red marrow (otherwise generally known as myeloid tissue) and yellow marrow. Red blood cells, platelets, and most white blood cells come up from within purple marrow. In yellow marrow a couple of white cells are made; nonetheless, this marrow is dominated by giant fat globules (producing its yellow appearance). There are a quantity of diseases that will involve the bone marrow, together with infection and malignancy. Imaging app Determination of skeletal age Throughout life the bones develop in a predictable way to type the skeletally mature adult on the finish of puberty. In western international locations, skeletal maturity tends to occur between the ages of 20 and 25 years. Typically, the nondominant (left hand) is radiographed and is compared with a collection of normal radiographs. Clinical app Bone fractures Fractures happen in normal bone because of abnormal load or stress, by which the bone provides method. In kids whose bones are still creating, fractures could happen across the growth plate or throughout the shaft. Clinical app Epiphyseal fractures As the skeleton develops, there are stages of intense progress usually across the ages of seven to 10 years and later in puberty. These development spurts are related to elevated cellular activity across the development plate and the metaphyseal region. This improve in exercise renders the growth plates and metaphyseal regions extra weak to injuries similar to dislocation across a progress plate or fracture by way of a development plate. Occasionally an injury may lead to development plate compression, destroying that area of the expansion plate, which can lead to asymmetric development. Clinical app Avascular necrosis Avascular necrosis is cellular death of bone resulting from a quick lived or everlasting lack of blood provide to that bone. A typical web site for avascular necrosis is a fracture throughout the femoral neck in an aged patient. Blood vessels that cross a joint and nerves that innervate muscle tissue appearing on a joint often contribute articular branches to that joint. Clinical app Osteoporosis Osteoporosis is a illness by which the bone mineral density is signi cantly reduced. Typically, osteoporotic fractures occur in the femoral necks, the vertebrae, and the wrists. Although osteoporosis could Synovial joints Synovial joints are connections between skeletal elements where the elements involved are separated by a slim articular cavity. In addition to containing an articular cavity, these joints have a quantity of characteristic options. First, a layer of cartilage, normally hyaline cartilage, covers the articulating surfaces of the skeletal elements. As a consequence, when these joints are viewed in normal radiographs, a wide gap seems to separate the adjacent bones because the cartilage that covers the articulating surfaces is extra clear to X-rays than bone. A second attribute characteristic of synovial joints is the presence of a joint capsule consisting of an inside synovial membrane and an outer brous membrane. The synovial membrane attaches to the margins of the joint surfaces at the interface between the cartilage and bone and encloses the articular cavity. The synovial membrane is extremely vascular and produces synovial uid, which percolates into the articular cavity and lubricates the articulating surfaces. Closed sacs of synovial membrane additionally occur outside joints the place they kind synovial bursae or tendon sheaths. Bursae usually intervene between constructions, corresponding to tendons and bone, tendons and joints, or skin and bone, and cut back the friction of one construction moving over the opposite. The brous membrane is shaped by dense connective tissue and surrounds and stabilizes the joint. Parts of the brous membrane could thicken to form ligaments, which further stabilize the joint. Another frequent however not universal characteristic of synovial joints is the presence of additional structures within the space enclosed by the capsule or synovial membrane: B Humerus Ulna Radius Synovial membrane 1 Articular discs (usually composed of brocartilage) take up compression forces, adjust to adjustments within the contours of joint surfaces throughout actions, and improve the vary of movements that may occur at joints. Fat pads occur between the synovial membrane and the capsule and move into and out of regions as joint contours change throughout motion; tendons. Descriptions of synovial joints based on form and movement Synovial joints are described based on shape and motion: Based on the shape of their articular surfaces, synovial joints are described as airplane (at), hinge, pivot, bicondylar (two units of contact points), condylar (ellipsoid), saddle, and ball and socket. Based on movement, synovial joints are described as uniaxial (movement in a single plane), biaxial (movement in two planes), and multiaxial (movement in three planes). Pivot joints-allow motion around one axis that passes longitudinally alongside the shaft of the bone; permit rotation. Sutures happen only within the skull where adjoining bones are linked by a thin layer of connective tissue termed a sutural ligament. In these joints, quick collagen tissue bers within the periodontal ligament run between the basis of the tooth and the bony socket. Examples are the ligamentum avum, which connects adjoining vertebral laminae, and an interosseus membrane, which links, for example, the radius and ulna in the forearm. Synchondroses happen the place two ossi cation centers in a developing bone stay separated by a layer of cartilage, for instance the expansion plate that happens between the pinnacle and shaft of developing lengthy bones. Body systems � Skin and fascias these joints permit bone development and ultimately turn into completely ossi ed. Most of most of these joints occur in the midline and include the pubic symphysis between the 2 pelvic bones, and intervertebral discs between adjoining vertebrae. Joints that have severely degenerated or lack their normal perform are painful, which may be life limiting, and in otherwise t and wholesome people can limit activities of day by day living. In some patients the ache may be so extreme that it prevents them from leaving the home and enterprise even the smallest of activities without discomfort. However, with ongoing developments in joint substitute materials and surgical strategies, even small joints of the ngers may be replaced. In the hip joint the acetabulum will be reamed, and a plastic or steel cup shall be introduced. Los s of joint s pa ce Clinical app Arthroscopy Ace ta bulum Artificia l fe mora l he a d. There are additional signi cant degenerative modifications within the left hip joint, which may even must be replaced. Arthroscopy is a method of visualizing the inside of a joint using a small digicam positioned via a tiny incision within the pores and skin. Arthroscopy can be carried out in most joints, including the elbow and wrist joints.