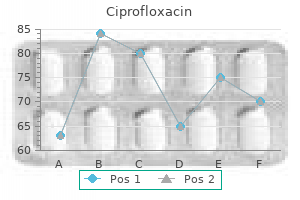
Ciprofloxacin dosages: 1000 mg, 750 mg, 500 mg, 250 mg
Ciprofloxacin packs: 30 pills, 60 pills, 90 pills, 120 pills, 180 pills, 270 pills, 360 pills

Ciprofloxacin 500 mg with visa
They move obliquely downwards and laterally antimicrobial underpants purchase 250 mg ciprofloxacin, parallel with the posterior borders of the external intercostals virus encrypted files ciprofloxacin 500 mg buy generic line. Each is hooked up to the upper edge and exterior floor of the rib instantly under the vertebra from which it takes origin, between the tubercle and the angle (levatores costarum breves). Each of the four lower muscles divides into two fasciculi; one is connected as already described, and the opposite descends to the second rib beneath its origin (levatores costarum longi). Innervation Levatores costarum are equipped by the lateral branches of the dorsal rami of the corresponding thoracic spinal nerves. Action Levatores costarum elevate the ribs but their significance in ventilation is disputed. They are additionally mentioned to act from their costal attachments as rotators and lateral flexors of the vertebral column. Innervation Internal intercostals are equipped by the adjacent intercostal nerves. Innermost intercostals the innermost intercostals had been once considered internal laminae of the internal intercostal muscle tissue, and fibres within the two layers do coincide in course. They are insignificant, and generally absent, on the highest thoracic levels however turn out to be progressively extra substantial beneath this, sometimes extending by way of the middle two quarters of the lower intercostal spaces. The innermost intercostals are associated internally to the endothoracic fascia and parietal pleura, and externally to the intercostal nerves and vessels. It arises by a skinny aponeurosis from the lower part of the nuchal ligament, the spines of the seventh cervical and higher two or three thoracic vertebrae, and their supraspinous ligaments. It descends laterally and ends in four digitations hooked up to the higher borders and external surfaces of the second, third, fourth and fifth ribs, just lateral to their angles. It is superficial to the thoracic a half of the thoracolumbar fascia and deep to the rhomboids. The number of digitations can differ from three to six, and the muscle may even be absent. Innervation Serratus posterior superior is innervated by the second, third, fourth and fifth intercostal nerves. Action the attachments of serratus posterior superior clearly indicate that it might elevate the ribs; its position in people is unsure. Innervation Innermost intercostals are provided by the adjoining intercostal nerves. Semispinalis capitis Mastoid process Splenius capitis Action Innermost intercostals are believed to act with the internal intercostals (Ch. Subcostales Innervation Subcostales are supplied by the adjacent intercostal nerves. It arises from the decrease third of the posterior floor of the sternum, the xiphoid process and the costal cartilages of the decrease three or four true ribs close to their sternal ends. The fibres diverge and ascend laterally as slips that cross into the lower borders and internal surfaces of the costal cartilages of the second, third, fourth, fifth and sixth ribs. The lowest fibres are horizontal and are contiguous with the highest fibres of transversus abdominis; the intermediate fibres are oblique; and the best are virtually vertical. Transversus thoracis varies in its attachments, not only between people but even on opposite sides of the same particular person. Like the innermost intercostals and subcostales, transversus thoracis separates the intercostal nerves from the pleura. External indirect Erector spinae tendon Gluteus medius Gluteus maximus Innervation Transversus thoracis is equipped by the adjoining intercostal nerves. Each descends from the inner surface of one rib, near its angle, to the inner surface of the second or third rib below. Their fibres run parallel to these of the interior intercostals and, just like the innermost intercostals, they lie between the intercostal vessels and nerves and the pleura. It arises from the spines of the lower two thoracic and higher two or three lumbar vertebrae and their supraspinous ligaments by a skinny aponeurosis that blends with the lumbar part of the thoracolumbar fascia. It ascends laterally and its four digitations cross into the inferior borders and outer surfaces of the lower 4 ribs, slightly lateral to their angles. There may be fewer digitations and, in rare instances, the whole muscle may be absent. It descends behind the first six costal cartilages, 1 cm from the lateral sternal border and divides on the level of the sixth intercostal space into musculophrenic and superior epigastric branches. Relations At first, the inner thoracic artery descends anteromedially behind the sternal end of the clavicle, the inner jugular and brachiocephalic veins, and the first costal cartilage. As it enters the thorax, the phrenic nerve crosses it obliquely from its lateral facet, often in front. The artery then descends virtually vertically to its bifurcation, mendacity behind pectoralis main, the first six costal cartilages, exterior intercostal membranes, internal intercostals and terminations of the upper six intercostal nerves. It is separated from the pleura, down to the second or third cartilage, by a robust layer of fascia, and below this by transversus thoracis. The artery is accompanied by a sequence of lymph nodes and by venae comitantes that unite at about the third costal cartilage right into a single vein medial to the artery. Innervation Serratus posterior inferior is innervated by ventral rami of the ninth, tenth, eleventh and twelfth thoracic spinal nerves. Action Serratus posterior inferior draws the decrease ribs downwards and backwards, although presumably not in ventilation. Sternalis Sternalis is an anatomical variation well known to anatomists but comparatively unknown to clinicians and surgeons (Snosek et al 2014). The muscle appears as a parasternal mass deep to the superficial fascia of the anterior thoracic wall and superficial to the pectoral fascia overlying pectoralis main. It could also be a cord-like, flat band or irregular and flame-like in shape, is type of twice as generally unilateral, and occurs more usually on the proper facet. Various attachment sites have been described in an extensive anatomical literature, together with the sternum, inferior border of the clavicle, sternocleidomastoid fascia, pectoralis major, and the higher ribs and their costal cartilages, all superiorly, and the lower ribs and their costal cartilages, pectoralis major, the rectus sheath and the exterior stomach oblique aponeurosis, all inferiorly. Its superficial location makes it an ideal candidate for utilization as a muscular flap in plastic reconstruction of the head and neck area. The aetiology is unknown; sternalis could also be an example of a a lot larger group of variations, including pectoralis minimus, pectoralis tertius, infraclavicularis and chondroepitrochlearis, which may be thought to be attributable to a disturbance of the traditional processes of pectoral muscle development. The relationship of sternalis to pectoralis major may cause a diagnostic dilemma throughout breast surgical procedure, mammography, computed tomography and magnetic resonance imaging scans as a result of its look mimics tumour pathology of the region. Sternal branches Sternal branches are distributed to transversus thoracis, the periosteum of the posterior sternal floor and the sternal purple bone marrow. These branches, together with small branches of the pericardiacophrenic artery, anastomose with branches of the posterior intercostal and bronchial arteries to type a subpleural mediastinal plexus. Anterior intercostal branches Anterior intercostal arteries are distributed to the higher six intercostal spaces. The anterior intercostals often arise from the inner thoracic artery as single vessels that promptly divide into two branches, one passing superiorly, the other inferiorly within each intercostal house. They supply the intercostal muscle tissue and send branches by way of them to the pectoral muscles, breast and skin.
Ciprofloxacin 500 mg purchase line
Tight and full closure ensues with the speedy decrease in ventricular strain in diastole bacteria 1000x magnification generic 500 mg ciprofloxacin mastercard. Commissures narrow natural antibiotics for acne treatment buy ciprofloxacin 250 mg mastercard, nodules combination and the valve reassumes its triradiate kind. Experiments point out that 4% of ejected blood regurgitates through a valve with regular sinuses, whereas 23% regurgitates via a valve without them. The regular construction of the aortic sinuses additionally promotes nonturbulent circulate into the coronary arteries. Aortic valve leaflets the aortic valve leaflets are connected partly to the aortic wall and in part to the supporting ventricular constructions. As with the pulmonary valve, the semilunar attachments incorporate segments of ventricular tissue within the bases of two of the aortic sinuses. However, the so-called non-coronary leaflet is better termed the non-adjacent leaflet as a outcome of it not often offers rise to a coronary artery. The semilunar attachments incorporate three triangular areas (trigones) of aortic wall throughout the apex of the left ventricular outflow tract. They are interposed between the bulbous aortic sinuses and separate the cavity of the left ventricle from the pericardial area. Removal of the trigones in an in any other case intact heart is instructive in demonstrating the relationships of the aortic valve, which, justifiably, could additionally be thought of as the keystone of the heart. The first triangle, between the non-coronary and left coronary leaflets, has a base continuous inferiorly with the fibrous aortic�mitral curtain. Although the basal attachments of each aortic valvular leaflet are thickened and collagenous at their ventricular origins, the leaflets lack a steady collagenous circular skeletal help; valvular perform relies upon primarily upon the semilunar attachments of the leaflets. With the valve half-open, each equals barely more than a quarter of a sphere, an approximate hemisphere being completed by the corresponding sinus. Angling the beam in path of the proper also allows assessment of the proper atrium, right ventricle and tricuspid valves. The hinge of the leaflet is nicely under the level of the ventriculoarterial junction. The muscular tissue of the ventricle is stained pink; fibrous tissue, which would show up as a attribute light colour with this stain, is absent. Note three aortic leaflets � right, left and non-adjacent � and the central position of the aorta. Note the totally different orientation compared with transthoracic echocardiography (looked at from under, foot to head). Rotation of the transducer allows two-chamber views of the heart and more detailed evaluation of the aorta and aortic valves. Over a lot of the heart, a nice layer of areolar tissue is discovered beneath the mesothelium of the serous (visceral) epicardium that accumulates subepicardial fat, concentrated along the acute margin, the atrioventricular and interventricular grooves, and their side channels. The coronary vessels and their major branches are embedded on this fat; the amount increases with age. Fibrocellular components of those subepicardial and subendocardial layers blend on their mural features with the endomysial and perimysial connective tissue on the myocardium. Each cardiac myocyte is invested by a fragile endomysium composed of nice reticular, collagen and elastin fibres embedded in floor substance. This matrix is missing solely at desmosomal and hole junctional contacts of intercalated discs. Similar preparations apply to ventricular conduction myocytes and their extensive working myocardial contacts. The 1012 connective tissue matrix itself is interconnected laterally to kind bundles, strands or sheets of macroscopic proportions displaying a complex geometric sample. Surrounding and attaching to larger myocardial bundles are stronger perimysial condensations. Running at the ventricular base is a posh framework of dense collagen with membranous, tendinous and fibroareolar extensions, intimately associated to atrioventricular valves and the aortic orifice. The leaflets of the pulmonary valve are supported on a free-standing sleeve of proper ventricular infundibulum that can easily be faraway from the center without disturbing either the fibrous skeleton or the left ventricle. Two pairs of curved, tapering, collagenous prongs, fila coronaria, lengthen from the central fibrous physique. They are stronger on the left, the place they pass partially around the mitral and tricuspid orifices. In contrast, the aortic valve faces superiorly, lying anterosuperior and to the best of the mitral orifice. The two ends of the curtain are strengthened as the right and left fibrous trigones, which are the strongest components of the skeleton. The proper trigone, together with the membranous septum, constitutes the central fibrous 7 Heart body, which is penetrated by the atrioventricular bundle of His (see below). The membranous septum is crossed on its proper facet by the attachment of the tricuspid valve, dividing the septum into atrioventricular and interventricular elements. However, as with the pulmonary valve, the construction of the aortic root corresponds to the triple fibrous semilunar attachments of its leaflets. Within this complex circumferential zone are three crucially important triangular areas that separate, on the ventricular facet, the aortic bulbous sinuses that home the valvular leaflets. As an entire, three triangles, known as the subaortic spans, can be conceptualized by method of a three-pointed coronet; their triangular apices correspond to the ideas of the valvular commissures and their walls, considerably thinner than those of the sinuses, consist variously of collagen or admixed muscle strands and fibroelastic tissue. The second span between the non-coronary and right coronary sinuses is continuous with the anterior surface of the membranous septum. The third span, between the two coronary aortic sinuses, is filled with loose fibroelastic tissue and separates the extension of the subaortic root from the wall of the free-standing subpulmonary infundibulum. Previously, this was thought to be the location of the tendon of the infundibulum (conal (conus) ligament) (Loukas et al 2007); analysis utilizing mouse hearts has proven that the ligament is found at the stage of the sinutubular junctions at the web site of preliminary fusion of the distal outflow cushions. The line of proximal fusion is the longitudinal raphe sometimes seen within the muscular subpulmonary infundibulum. Similar fibrous triangles are discovered separating the sinuses of the pulmonary trunk however these are considerably less sturdy. The straight fringe of the tricuspid valve represents the attachment of the septal leaflet, marking the inferior border of the triangle of Koch, and the rest supports the anterosuperior and inferior leaflets. At a quantity of websites, solely fibroareolar tissue separates the atrial and ventricular muscular lots. The fibrous skeleton ensures electrophysiological discontinuity between the atrial and ventricular myocardial plenty (except at the website of penetration of the conduction tissue). It additionally offers direct attachment for the myocardium and for fibrous tissue all through the center as a support matrix for a three-dimensional meshwork of cardiomyocytes. The tracks are created from the primary eigenvectors and symbolize the alignment of the aggregated myocytes. This approach permits the identification of reproducible tracks, or pathways, through the myocardium that join distant finish and epicardial regions via simultaneous modifications in helical and intrusion angles. Only a small proportion of the anomalies are immediately attributable to genetic or environmental elements and the bulk are the outcomes of multifactorial occasions. Ventricular myocytes kind a three-dimensional mesh in a supporting fibrous matrix.
Diseases
- Hyperlipoproteinemia type II
- Tetraamelia pulmonary hypoplasia
- Hyperornithinemia, hyperammonemia, homocitrullinuria syndrome
- Legionellosis
- Non-small cell lung cancer
- Macrocephaly pigmentation large hands feet
- Pseudohermaphrodism anorectal anomalies
- Procrastination
- Meinecke Pepper syndrome
Generic 1000 mg ciprofloxacin otc
The presence of the uterus and vagina means that there are two pelvic pouches instead of the one rectovesical pouch seen in males infection game strategy ciprofloxacin 1000 mg with mastercard. The peritoneum from the rectum is mirrored anteriorly on to the posterior floor of the posterior fornix of the vagina and the uterus bacteria 10 safe 750 mg ciprofloxacin, forming the recto-uterine pouch (of Douglas). The depth of the pouch � particularly, the extent to which it descends on the posterior floor of the vagina � is variable (Baessler and Schuessler 2000). As in males, the peritoneum over the dome of the bladder is reflected on to the posterior surface of the lower anterior belly wall. Recto-uterine folds containing the uterosacral ligaments cross posteriorly from the edges of the cervix to the sacrum, working lateral to the rectum. This consists of anterior and posterior layers which might be steady at the upper border of the ligament. The broad ligament accommodates the uterine tubes in its free higher border; the ovaries are suspended from its posterior layer. The ovarian fossa is a shallow depression within the peritoneal lining of the lateral pelvic wall between the peritoneal ridges formed by the obliterated umbilical arteries anteriorly, the ureter posteriorly, and the exterior iliac vessels above; it lies behind the lateral attachment of the broad ligament and often incorporates the ovary in nulliparous females. Parietal peritoneum is provided by the somatic blood vessels of the abdominal and pelvic walls, and its lymphatics be part of those in the physique wall and drain to parietal lymph nodes. Visceral peritoneum is finest thought of as an integral part of the viscus it covers: its blood supply and lymphatic drainage subsequently correspond to those of the associated viscus. Pain from the pancreas, gallbladder and even the small bowel might radiate to the back. Stretch or irritation of the visceral peritoneum may also elicit profound reflex vasomotor and cardiac changes mediated by autonomic nerves, together with a vasovagal response. Painful responses to manipulation of the parietal peritoneum may be abolished by native or regional anaesthesia. In marked contrast, the direct central connections of visceral afferents, significantly through the vagus nerve, imply that stretching the visceral peritoneum may induce profound results, including acute haemodynamic instability, regardless of local or regional (including spinal) anaesthesia. It consists of the larger sac, which is the primary peritoneal cavity surrounding many of the stomach and pelvic viscera, and the lesser sac, or omental bursa, which is a small diverticulum situated behind the stomach and lesser omentum and in entrance of the pancreas. It is beneficial to divide the peritoneal cavity into two primary compartments, supramesocolic (often simply referred to as supracolic) and inframesocolic (or infracolic), which are partially separated by the transverse colon and its mesentery. The visceral peritoneum is innervated by afferent nerves that travel with the autonomic provide to the underlying viscera. Sensations arising from pathologies that have an result on the parietal or visceral peritoneum replicate these different patterns of innervation. Well-localized ache is elicited by mechanical, thermal or chemical stimulation of nociceptors within the parietal peritoneum; the pain is normally properly localized to the affected region. Somatic nerves that innervate the parietal peritoneum additionally provide the corresponding segmental skin and muscle tissue; when the parietal peritoneum is irritated, local reflex muscle contraction occurs, resulting in clinical indicators of guarding and even rigidity of the abdominal wall. The parietal diaphragmatic peritoneum is provided centrally by afferent fibres from the phrenic nerves and peripherally by the decrease intercostal and subcostal nerves; peripheral irritation of the diaphragm could due to this fact result in pain localized in the distribution of the lower thoracic spinal nerves, while central irritation causes referred pain in the cutaneous distribution of the third to fifth cervical spinal nerves (the shoulder region). The innervation of the parietal peritoneum of the true pelvis is poorly documented however the obturator nerve makes a big contribution. Irritation or stretch of the visceral peritoneum causes poorly localized discomfort. The proper supramesocolic area could be subdivided into the proper subphrenic area, the best subhepatic house and the lesser sac. The left supramesocolic area could be divided into two subspaces: the left subphrenic house and the left perihepatic space. Right subhepatic space (hepatorenal pouch) the best subhepatic house lies between the inferior floor of the best lobe of the liver and the higher pole of the best kidney. It is bounded superiorly by the inferior layer of the coronary ligament, laterally by the right lateral stomach wall, posteriorly by the anterior surface of the upper pole of the best kidney, and inferomedially by the hepatic flexure, transverse mesocolon, second part of the duodenum, and part of the top of the pancreas. In the supine place, the hepatorenal pouch (of Morison) is extra dependent than the best paracolic gutter. Lesser sac (omental bursa) the lesser sac is a cavity lined with peritoneum and connected to the principle peritoneal cavity (greater sac) by the epiploic foramen (of Winslow). It is taken into account a half of the proper supramesocolic compartment because it develops in the embryo on the right side of the ventral mesogastrium (p. It has posterior and anterior walls and superior, inferior, proper and left borders. The sac varies in measurement based on the amount of the viscera making up its partitions; it might be partially obliterated by pure adhesions between the anterior and posterior walls. At its right border, the anterior wall is mostly formed by the lesser omentum but, towards the left, the lesser omentum becomes progressively shorter and more of the anterior wall is shaped by the posterior surface of the stomach and greater omentum. The lower part of the posterior wall of the lesser sac is shaped by the anterior peritoneal layer of the posterior sheet of the larger omentum, which overlies the transverse mesocolon. The inferior phrenic, splenic, left gastric and common hepatic arteries lie partly behind the bursa. Here, the peritoneum of the posterior wall of the lesser sac is mirrored anteriorly from the diaphragm to be a part of the posterior layer of the lesser omentum. The inferior border runs along the road of fusion of the layers of the higher omentum, which extends from the gastrosplenic ligament on the left to the peritoneal fold behind the primary part of the duodenum on the proper. The proper border of the lesser sac is where the peritoneum overlying the head and neck of the pancreas is mirrored on to the inferior aspect of the first a part of the duodenum. The line of this reflection ascends to the left, along the medial aspect of the gastroduodenal artery. Near the upper duodenal border, the proper border joins the floor of the epiploic foramen round the hepatic artery correct. Above the epiploic foramen, the right border is formed by the peritoneal reflection from the diaphragm to the best margin of the caudate lobe of the liver, which then crosses the inferior vena cava. The a part of the lesser sac mendacity between the splenorenal and gastrosplenic ligaments is referred to as the splenic recess. Above the spleen, the two ligaments merge to form the brief gastrophrenic ligament, which passes forwards from the diaphragm to the posterior facet of the fundus of the stomach and varieties part of the upper left border of the lesser sac. The two layers of the gastrophrenic ligament diverge close to the belly oesophagus, leaving a part of the posterior gastric surface devoid of peritoneum. The lesser sac is indented by a crescentic peritoneal fold that runs from the higher border of the neck of the pancreas to the higher a part of the lesser curvature of the stomach. The upper a part of this fold overlies the left gastric artery as it runs from the posterior abdominal wall to the lesser curvature of the stomach. The decrease part of the fold overlies the widespread hepatic artery because it runs from the posterior abdominal wall to the lesser omentum. When the fold is outstanding, it divides the lesser sac right into a smaller superior and a bigger inferior recess.
250 mg ciprofloxacin cheap overnight delivery
By 34 days of gestation antibiotic resistance patterns ciprofloxacin 1000 mg cheap without a prescription, blood circulates from the aortic sac via pulmonary arteries right into a capillary plexus around the two lung buds and drains to the growing atrium infection 2 strategy generic ciprofloxacin 500 mg line. As every new airway forms in the mesenchyme, a new plexus types as a halo around it and coalesces with the vessels already alongside the previous airway. In this way, addition of the newly formed tubules to the present vessels is sustained; the airways act as a template for the event of blood vessels. Initially, this arterial tunica media is derived from the bronchial smooth muscle of the adjacent airways, however because the vessels progressively enlarge, cells derived from the splanchnopleuric mesenchyme differentiate around the wall to form layers of smooth muscle cells. The muscular wall is thick relative to the lumen and this, partly, will increase resistance to blood flow, although only 10% of blood circulate goes by way of the pulmonary circulation of the lung during intrauterine life. None the much less, this small blood move is important in normal lung improvement (see below). Vascular innervation follows muscularization; the vasoactive peptides within the nerves are predominantly vasoconstrictor. As the pulmonary veins enlarge, they become separated from the airways by lymphatic vessels mendacity within connective tissue. At around week 12, the peripheral veins develop a single layer of smooth muscle cells of their walls. This layer is derived solely from the splanchnopleuric mesenchyme and not from bronchial clean muscle (as occurs within the arteries). The lumen of every vein is comparatively giant and the wall is comparatively thin in any respect ranges. Arteries and veins proceed to develop in the canalicular phase, most likely by angiogenesis; dividing cells are seen within the peripheral capillaries. The epithelium of the most peripheral conducting airways flattens when the developing capillaries come to lie immediately subjacent to it during this part. Two or three bronchial arteries develop from the descending aorta from week 8 onwards, entering the lung on the hilum. These arteries extend down the intrapulmonary airways, ultimately forming subepithelial and adventitial plexuses, which, by birth, have reached the distal parts of the bronchioli. Saccular/alveolar part (28 weeks to term: first look of alveoli in humans) Thin-walled terminal saccules are obvious on the saccular stage and will become alveolar ducts as development proceeds. The growth of the potential respiratory airspaces that occurs throughout this period is accompanied by an extra lower in the amount of interstitial tissue, and the capillary networks turn out to be ever more intently against the pneumocyte epithelium. As a crest protrudes into a saccule, a half of the capillary network turns into drawn into it. After the later expansion of the saccules on all sides of the crest, a double capillary layer turns into annexed between what are actually alveolar partitions. During the saccular stage, elastin is deposited beneath the epithelium (an important step for future alveolar formation), and surfactant manufacturing from type 2 pneumocytes (essential for the survival of a preterm neonate) matures. Maturation of the blood�gas barrier is an essential part of normal human development but the molecular basis of that is little understood. The distal airspaces broaden throughout late gestation and continue to do so after delivery. The variety of alveoli current at birth (variously estimated as between none and 5 � 107) is controversial but the numbers probably increase significantly quickly over the primary 6 months of life. The alveolar stage is now considered to continue beyond infancy and to final throughout childhood (see below). The formation of millions of alveoli is completed by a complex process of folding and division. Existing partitions of distal airspaces become thinner as pneumocyte epithelial cells flatten, and some cells bear apoptosis. Ridges subsequently develop out from the sides of the saccule walls, forming primitive alveoli. The secondary septa contain a double capillary layer and further new alveoli form by the infolding of certainly one of these layers, additional subdividing the airspaces. The double capillary networks then bear remodelling to kind the acquainted single capillary sheet around each alveolus. Conducting airways also bear profound postnatal adjustments and exhibit elevated smooth muscle and bronchoconstrictor responsiveness. This experimental finding implies that iatrogenic damage to the creating alveoli when ventilating a preterm baby with oxygen- 927 Chapter fifty two Development of the thorax the bronchial veins from the periphery of the lungs drain into the pulmonary veins. Bronchial arteries also provide the pleura close to the hilum, and kind vasa vasorum within the adventitia of the large arteries and veins. Postnatally, inflammatory lung conditions, similar to bronchial asthma, cystic fibrosis and bronchiectasis, trigger hypertrophy of the bronchial circulation and these vessels may bleed, typically giving rise to huge haemoptysis (see McCullagh et al (2010)). Both circumstances are inclined to remit over time, and in neither case is it identified whether the abnormal cells are of pathophysiological significance or are merely markers of another course of. Intrauterine maturation of the lungs There are greater than 30 totally different cell sorts within the adult lung that mature throughout improvement. Pulmonary surfactant is produced by kind 2 alveolar epithelial cells and saved in lamellar bodies. Surfactant proteins (Sp) B and C are surface-active, whereas A and D are a part of the collectin family of pattern recognition receptors. Surfactant is crucial for sustaining the functional integrity of alveoli; the principle morbidity of utmost prematurity displays surfactant deficiency inflicting neonatal respiratory distress (treatment of these infants has been reworked by the supply of exogenous surfactant). Fetal respiration movements appear to be important in surfactant synthesis: the practical maturation of the surfactant system could be accelerated therapeutically by the administration of steroids to the mother. Normal lung development requires adequate intrathoracic space, normal fetal respiratory actions and adequate amniotic fluid. There is evidence that perturbation of fetal lung blood flow additionally impacts lung growth, even though a lot of the right ventricular output of the heart is shunted away from the lungs by way of the ductus arteriosus; pulmonary valve stenosis is related to pulmonary hypoplasia. Lung progress becomes impaired by restricted growth, and distension of the developing lung could provide a significant stimulus to development during regular growth. Absence or impairment of fetal breathing actions, and anomalies affecting diaphragmatic exercise, are all associated with pulmonary hypoplasia. It is believed that standard fetal breathing actions improve the lung quantity and stimulate growth of the distal airspaces. The relationship between lung fluid and amniotic fluid is much extra complicated than was beforehand believed. In renal agenesis, lowered bronchial branching occurs as early as 12�14 weeks of gestation. Later, the presence of amniotic fluid is important for normal fetal lung growth. The fetal lung is a web fluid secretor, the output of fluid reaching as excessive as 5 ml/kg shortly before delivery (see p.
Purchase 250 mg ciprofloxacin amex
The bones are united by articular capsules and by dorsal antibiotics for recurrent uti in pregnancy discount 1000 mg ciprofloxacin free shipping, palmar and interosseous ligaments virus hitting us ciprofloxacin 750 mg order mastercard. The second to fifth carpometacarpal joints exhibit an increasing vary of movement, progressing from the radial to the ulnar facet. The second metacarpal has two ligaments, from the trapezium and trapezoid; the third has two, from the trapezoid and capitate; the fourth has two, from the capitate and hamate; and the fifth has a single band from the hamate, which is steady with an analogous palmar ligament, forming an incomplete capsule. The palmar ligaments are comparable, besides that the third metacarpal has three: a lateral from the trapezium, superficial to the tendon sheath of flexor carpi radialis, an intermediate from the capitate, and a medial from the hamate. They are restricted to one a part of the carpometacarpal articulation and join contiguous distal margins of the capitate and hamate with adjoining surfaces of the third and fourth metacarpal bones; they could be united proximally. Wrist and hand Some degree of carpal instability could happen as a part of inherent hypermobility in affected individuals. When axially loaded, the distal row of the carpus compresses the proximal row, causing the scaphoid to rotate into flexion and pronation. Provided the scapholunate and lunotriquetral ligaments remain intact, the load is transmitted to the lunate and triquetrum. In the proximal row, the scaphoid exhibits the best vary of motion, the lunate less and the triquetrum the least. Consequently, the scapholunate and lunotriquetral ligaments tighten as the scaphoid is progressively flexed, thereby growing the intrinsic stability of the proximal row. Occasionally, the joint between the hamate and fourth and fifth metacarpal bones has a separate synovial cavity, bounded laterally by the medial interosseous ligament and its extensions to the palmar and dorsal elements of the capsule. Muscles producing movements Slight gliding actions are effected by the long flexor and extensor muscle tissue of the digits. Collateral ligament (fan-like part) Volar plate Metacarpal Fibrous capsule the intermetacarpal joints have fibrous capsules. The interosseous ligaments join contiguous surfaces just distal to their articular aspects. Synovial membranes the synovial membranes are steady with those of the carpometacarpal articulations. Movements on the carpometacarpal and intermetacarpal joints Movements on the carpometacarpal and intermetacarpal articulations are restricted to slight gliding, enough to permit some flexion� extension and adjunct rotation; ranges range in numerous joints. The fifth metacarpal is most movable and the second and third are the least cell. These variations are easily demonstrated by opposing every digit to the thumb over the palmar centre. About two-thirds of the actions are these of the thumb, as described above, however during opposition, the carpometacarpal and metacarpal joints of the little finger become flexed, kidnapped and laterally rotated, accounting for the remaining third of the motion. A further accessory motion is spiral twisting of the whole metacarpus on the carpus. Collateral ligaments the collateral ligaments are strong, spherical cords that flank the joints. Synovial membrane the metacarpophalangeal joints are lined by a synovial membrane. The range of rotation is regularly elevated as a outcome of the resistance of a grasped object. Active flexion is 90� or more, whereas extension ranges from 10� (index) to 30� (little); both movements are limited principally by antagonistic muscles. The metacarpophalangeal joint of the thumb has a flexion�extension vary of roughly 60�, which is almost totally flexion. Flexion of the index finger may be accompanied by minimal lateral rotation or no rotation; a small diploma of medial rotation is regularly noticed. Other movements are adduction�abduction (maximal vary 25�), which invariably accompanies the corresponding carpometacarpal actions and will increase their combined range; and slight rotation, which accompanies flexion� extension. Of the second to fifth metacarpophalangeal joints, the second is most mobile in adduction�abduction (approximately 30�), followed by the fifth, fourth and third. Ligaments Each metacarpophalangeal joint has a palmar and two collateral ligaments. They are thick, dense and fibrocartilaginous, and are sited between, and related to , the collateral ligaments. Their palmar aspects are blended with the deep transverse palmar ligaments and are grooved for the flexor tendons, whose fibrous sheaths join with the edges of the grooves. Deep transverse metacarpal ligaments the deep transverse metacarpal ligaments are three short, broad, flat bands that join the palmar ligaments of the second to fifth metacarpophalangeal joints. They are related anteriorly to the lumbricals and digital vessels and nerves, and posteriorly to the interossei. Bands from the digital slips of the central palmar aponeurosis join their palmar surfaces. On each side of the third and fourth metacarpophalangeal joints, however solely the ulnar aspect of the second and radial side of the fifth joints, transverse bands of the dorsal digital expansions be part of the deep transverse metacarpal ligaments. Accessory movements Accessory movements are additional rotation (most marked within the thumb), anteroposterior and lateral translation of a phalanx or metacarpal, and distraction. Muscles producing movements the muscular tissues producing actions on the metacarpophalangeal joints are as follows. Flexion Flexion is produced by flexors digitorum superficialis and profundus, assisted by the lumbricals, interossei and flexor digiti minimi brevis (in the little finger). In the thumb, flexors pollicis longus and brevis, and the primary palmar interosseous, are involved. Extension Extension is produced by extensor digitorum, assisted within the second and fifth digits by extensor indicis and extensor digiti minimi, respectively. Adduction In extended fingers, adduction is produced by the palmar interossei; the long flexors are predominant throughout flexion. Abduction In extended fingers, abduction is produced by the dorsal interossei, assisted by the long extensors (except in the center finger), and abductor digiti minimi in the minimus. In the thumb, abductor pollicis brevis (which additionally contributes to opposition) is involved. When the fingers are flexed on the interphalangeal joints, lively abduction is restricted (it is virtually zero when metacarpophalangeal and interphalangeal joints are flexed); if the lengthy digital flexors are inactive, passive abduction is free. Inability to abduct actively in this position may be because of shortening of the dorsal interossei and abductor digiti minimi by flexion, but the altered line of pull of the interossei relative to the axis of motion might be the figuring out issue. Collateral ligaments the collateral ligaments move from the lateral aspect of the head of 1 phalanx to the volar side of the bottom of the adjoining phalanx. An accent part to the collateral ligament arises in continuity with the main ligament and passes in a volar course to connect to the volar plate. Factors maintaining stability Stability is conferred by the articular contours of the joint surfaces and the collateral ligaments. The flexor and extensor tendons and retinacular ligaments present secondary stabilization. Extensions from the extensor enlargement, every collateral ligament and the palmar ligament all move into the joint cavity and supply a major increase to the articular surface area of the phalangeal base; their deformable nature improves joint congruence. Joint actions Active actions on the interphalangeal joints are flexion and extension, and are larger in range on the proximal joints.
Syndromes
- Problems with sexual intercourse
- Blood loss
- Drowsiness
- Urinary tract infection
- Fatigue
- Has anyone in your life recently passed away?
Purchase ciprofloxacin 250 mg with mastercard
Diaphragmatic paralysis can be assessed by ultrasound examination with a sniff manoeuvre antibiotic induced colitis ciprofloxacin 500 mg purchase without prescription. Electrodes are placed adjacent to the nerves treatment for dogs diabetes cheap ciprofloxacin 500 mg overnight delivery, generally within the neck but more usually in the chest, and a ventilatory rhythm is established by trains of stimuli delivered by an implanted system. The diaphragm is the major muscle of inspiration, liable for approximately two-thirds of quiet inhaling wholesome people. The external intercostal muscular tissues are most active in inspiration, and the less sturdy inner intercostals in expiration. Increasing the vertical, transverse and anteroposterior dimensions of the chest will increase the amount of the pleural area, and the resulting decrease in intrapleural pressure draws air into the lungs. Air is expelled from the lungs and the elastic recoil of the lung creates a subatmospheric stress that returns the lateral and anteroposterior dimensions of the thorax to normal (De Troyer and Estenne 1988, Celli 1998). During inspiration, essentially the most inferior ribs are fixed and contraction of the diaphragm draws the central tendon inferiorly, scarcely altering diaphragmatic curvature. The cupulae move inferiorly and slightly anteriorly, virtually parallel to their unique positions. The associated inferior displacement of the belly viscera is permitted by the extensibility of the belly wall, however the restrict of this extensibility is quickly reached. The central tendon, its movement arrested by the belly viscera, then becomes a onerous and fast level from which the fibres of the diaphragm proceed to contract. The medial side of the rib is elevated and this increases the transverse dimension of the chest in the same method as a bucket handle swinging outwards; this effect is most evident within the inferior seventh to tenth ribs. The right cupula of the diaphragm, which lies on the liver, has a larger resistance to overcome than the left, which lies over the abdomen, and so the best crus and the fibres of the proper facet are extra substantial 974 than those of the left. The thoracic component is often extra marked in females, however will increase in both sexes during deep inspiration. Radiographs present that the peak of the diaphragm throughout the thorax also varies considerably with posture. It is highest when the physique is supine, when it performs the greatest ventilatory excursions with normal breathing. When the physique is erect, the diaphragm is decrease and its ventilatory actions become smaller. The diaphragmatic profile remains to be lower in the sitting posture and ventilatory excursions are smallest underneath these situations. The uppermost half sinks to a decrease level than that seen when sitting, and moves little with ventilation. The lower half rises higher within the thorax than it does even within the supine position, and its ventilatory excursions are considerably higher. Changes within the stage of the diaphragm with alterations in posture clarify why sufferers with severe dyspnoea are most comfy, and least in want of breath, when sitting up. After forced expiration, the proper cupula of the diaphragm is level anteriorly with the fourth costal cartilage, laterally with the fifth, sixth and seventh ribs, and posteriorly with the eighth rib; the left cupula is slightly lower. The ventilatory muscular tissues should also work throughout sleep, when the pharyngeal muscular tissues chill out and higher airway resistance increases. It can be clear that though ventilatory muscular tissues not often tire in normal life, they do fatigue when positioned beneath irregular loads. In quiet ventilation, the juxtahilar a half of the lung scarcely moves and the middle area moves only slightly. The primary position of the intercostal muscle tissue is to stiffen the chest wall, stopping paradoxical movement throughout inspiratory diaphragmatic descent. Immediately after high spinal injury, the important capacity decreases to about 300 ml, even though the diaphragm is transferring maximally, as a end result of some 2. Usually after a number of weeks, the paralysis turns into spastic, stiffening the chest wall, and the very important capacity will increase in direction of its phrenic limit of about 3 litres. In the same method, high spinal injury reveals the function of the stomach in inspiration and expiration. During the flaccid stage of high spinal paralysis, the only mechanisms obtainable for returning the relaxed diaphragm into the thorax on expiration are passive recoil of the lungs and chest wall, and the weight of the belly viscera. Conversely, when paralysis becomes spastic, the stiff stomach wall opposes inspiration. Loukas M, du Plessis M, Shah S et al 2015a the scientific anatomy of the musculotendinous part of the diaphragm. The superior mediastinum transmits the sympathetic and parasympathetic cardiac nerves, the phrenic nerve laterally, the vagus nerves medially and the left recurrent laryngeal nerve. The terminal a part of the thoracic duct emerges from the posterior side of the aorta and oesophagus, ascending between the left subclavian and carotid arteries. The superior (extrapericardial) half of the superior vena cava and its main tributaries are located on a extra superficial aircraft posterior to the manubrium and the origins of sternothyroid inferiorly, and sternohyoid superiorly. An enlarged thyroid gland may prolong inferiorly between the sternum and the brachiocephalic veins; its surgical excision requires due diligence from potential venous adherence. The origins of longus colli (inferior oblique and vertical intermediate portions) are the deepest components of the superior mediastinum. Strictly talking, the mediastinum is the visceral compartment between the 2 lungs and consists of the mediastinal pleura. It communicates with the neck via the superior thoracic aperture and with the extraperitoneal, extrapleural and epidural spaces. Beyond each pulmonary hilum, the mediastinum merges into the lung interstitium, incorporating the bronchial tree with its accompanying neurovascular bundles and the pulmonary vasculature. The posterior mediastinal boundary is longer because of the indirect disposition of the superior thoracic aperture and the diaphragmatic curvature posteroinferiorly. Detailed accounts of mediastinal contents are included with descriptions of the respiratory organs (Ch. The reflection of the costomediastinal pleurae follows a line that passes from the sternoclavicular joints in an inferomedial direction, to join the midline on the posterior facet of the sternal angle. It narrows above the fourth costal cartilages the place the pleural sacs converge, and accommodates unfastened connective tissue, the sternopericardial ligaments, a number of lymph nodes, the mediastinal branches of the internal thoracic artery, and generally part of the thymus gland or its degenerated stays. The pericardium and the guts are routinely approached by either a whole median or partial sternotomy. The sternopericardial ligaments and the pleural reflections are simply separated by blunt dissection. In case of pericardial tamponade, the pericardial cavity can be easily drained through a subxyphoid approach, both surgically or by way of needle pericardiocentesis. The quick thoracic a half of the inferior vena cava, each extra- and intrapericardial segments, extends between the vena caval aperture of the diaphragm and its termination in the best atrium. The mediastinal pleura is steady with the visceral pleura at the stage of the hilum, which is the place the lateral boundary of the center mediastinum is conventionally located.
Buy generic ciprofloxacin 750 mg online
The interventricular grooves prolong from the atrioventricular groove to the apical notch on the acute margin generic antibiotics for sinus infection 250 mg ciprofloxacin order mastercard, the latter a little to the best of the true cardiac apex antibiotic herbs 250 mg ciprofloxacin order. It faces posteriorly and to Heart the proper, separated from the thoracic vertebrae (fifth to eighth in the recumbent, sixth to ninth within the erect posture) by the pericardium, proper pulmonary veins, oesophagus and aorta. It extends superiorly to the bifurcation of the pulmonary trunk and inferiorly to the posterior a half of the atrioventricular groove, which incorporates the coronary sinus and coronary arterial branches. It is restricted to the right and left by the rounded surfaces of the corresponding atria, separated by the shallow interatrial groove. The level of junction of the atrioventricular, interatrial and posterior (inferior) interventricular grooves is termed the cardiac crux. Two pulmonary veins on each side open into the left atrial part of the base, whereas the superior and the inferior venae cavae open into the higher and decrease parts of the right atrial basal region. This description of the anatomical base displays the same old position of the center within the thorax. Such descriptions, while lower than good anatomically, will nearly definitely persist. Only a small a part of the left atrial appendage tasks forwards to the left of the pulmonary trunk. Of the ventricular area, about one-third is made up by the left and two-thirds by the best ventricle. The site of the septum between them is indicated by the anterior interventricular groove. The sternocostal surface is separated by the pericardium from the body of the sternum, the sternocostal muscles and the third to sixth costal cartilages. Because of the bulge of the heart to the left, extra of this floor is behind the left costal cartilages than the proper. It can also be lined by the pleural membranes and the thin anterior edges of the lungs, apart from a triangular area on the cardiac incisure of the left lung. The lungs and their pleural coverings are variable of their diploma of cardiac overlap. It is shaped by the ventricles (chiefly the left) and rests primarily on the central tendon but in addition, apically, on a small space of the left muscular a half of the diaphragm. It is separated from the anatomical base by the atrioventricular groove, and is traversed obliquely by the posterior (inferior) interventricular groove. Left surface of the heart Facing posterosuperiorly to the left, the left surface consists nearly entirely of the obtuse margin of the left ventricle, however a small part of the left atrium and its left atrial appendage contribute superiorly. It is separated by the pericardium from the left phrenic neurovascular bundle, and by the left pleura from the deep concavity of the left lung. Anatomical apex of the guts this is the apex of the conical left ventricle, which is directed anteroinferiorly and to the left. The apex is positioned mostly behind the fifth left intercostal area, near or somewhat medial to the midclavicular line. It consists of an atrial space superior and to the best, and a ventricular part inferior and to the left of the atrioventricular groove. The atrial space is occupied almost entirely by the right Right floor of the center the proper floor is rounded and shaped by the right atrial wall. It is separated from the mediastinal aspect of the right lung by the pericardium and pleural coverings. Its convexity merges inferiorly into the brief intrathoracic part of the inferior vena cava and above into the superior vena cava. The manubrium sterni has been retracted cranially, the thymus has been utterly eliminated and the pericardium has been partially removed. The hilum of the lung has been dissected to expose the tracheobronchial lymph nodes. The junction between the venous part (sinus venosus) and the atrium proper is marked externally by a shallow groove, the sulcus terminalis, extending between the right sides of the openings of the two venae cavae. The sulcus terminalis corresponds, internally, to the terminal crest (crista terminalis), which is the site of origin of the intensive pectinate muscles that arise serially at proper angles from the crest. Laterally, the atrium is also related to the mediastinal surface of the proper lung, however anterior to its hilum and separated from it by the pleura, right phrenic nerve and pericardiacophrenic vessels and pericardium. Posteriorly and to the left, the interatrial septum and the encompassing infolded atrial walls separate the atria (the mural infolding is indicated by an intensive interatrial groove). Medially are the ascending aorta and, to a limited extent, the pulmonary trunk and its bifurcation. Right border of the center Corresponding to the proper atrium, the profile of the right border is slightly convex to the best because it approaches the vertical. Inferior border of the guts Also generally identified as the acute margin of the center, the inferior border is sharp, skinny and practically horizontal. It extends from the lower limit of the best border to the apex and is formed primarily by the best ventricle, with a small contribution from the left ventricle near the apex. Left border of the center Also often known as the obtuse margin, the left border separates the sternocostal and left surfaces. It is round and mainly formed by the left ventricle but, to a slight extent superiorly, is fashioned by the left atrial appendage. It descends obliquely, convex to the left, from the appendage to the cardiac apex. Its walls kind the best superior sternocostal floor, the convex right (pulmonary) surface and somewhat of the right side of the anatomical base. The wall of the vestibule is easy however its junction with the appendage is ridged all around the atrioventricular junction by pectinate muscle tissue. The smooth-walled systemic venous sinus receives the openings of the venae cavae and coronary sinus; it originates from the sinus venosus of the embryonic heart. B, the triangle of Koch, outlined by the tendon of Todaro, orifice of the coronary sinus and the septal leaflet of the tricuspid valve. The superior and inferior venae cavae have been dissected, exposing the venous element of the proper atrium and the fossa ovalis. The superior vena cava returns blood from head, neck and upper limb via an orifice that faces anteroinferiorly and has no valve; it additionally receives blood from the chest wall and the oesophagus via the azygos system. It drains blood from all buildings beneath and together with the diaphragm into the bottom a part of the atrium near the septum. When traced inferiorly, it forms the Eustachian ridge, which runs into the sinus septum (see below), continuous with the valve of the coronary sinus. The lateral part of the valve turns into continuous with the decrease end of the terminal crest. The Eustachian valve is large during fetal life, when it serves to direct richly oxygenated blood (from the placenta) from the best atrium by way of the foramen ovale of the interatrial septum into the left atrium. It is usually guarded by a thin, semicircular Thebesian valve that covers the lower a half of the orifice. The higher limb of this valve joins the Eustachian valve and its muscular extension, the Eustachian ridge. It additionally joins a tendinous construction, the tendon of Todaro, running from this commissure into the sinus septum, which is the septum between the coronary sinus and the fossa ovalis. The tendon of Todaro runs forwards to insert into the central fibrous physique and is among the landmarks of the triangle of Koch (see below).
Ciprofloxacin 750 mg discount online
The sheaths around the thumb and little finger are steady with the flexor sheaths in entrance of the wrist virus japanese movie 500 mg ciprofloxacin order with amex. The parietal synovial membrane is mirrored on to the surface of the flexor tendon virus 96 ciprofloxacin 250 mg effective, forming a visceral synovium. A normal nomenclature for the anular (A) and cruciform (C) pulleys is used (Doyle and Blythe 1975). The A1 pulley is located anterior to the palmar cartilaginous plate of the metacarpophalangeal joint and may extend over the proximal a half of the proximal phalanx. It is the strongest pulley and arises from well-defined longitudinal ridges on the palmar side of the phalanx. A pouch or recess of synovium extends superficial to the free edge of the pulley fibres so that the free edge forms a lip protruding into the synovial area. A4 overlies the center third of the middle phalanx, and A5 overlies the distal interphalangeal joint. The tendons of abductor pollicis longus and extensor pollicis brevis lie in a tunnel on the lateral side of the styloid means of the radius; there could additionally be a separate synovial sheath for each, or the tendon of the abductor may be double. The tendons of extensors carpi radiales longus and brevis lie behind the styloid process; the tendon of extensor pollicis longus lies on the medial aspect of the dorsal tubercle of the radius; the tendons of extensors digitorum and indicis lie in a tunnel on the medial facet of the tubercle; the tendon of extensor digiti minimi lies opposite the interval between the radius and ulna; and the tendon of extensor carpi ulnaris lies between the head and the styloid strategy of the ulna. The tendon sheaths of abductor pollicis longus, extensors pollicis brevis and longus, extensors carpi radiales and extensor carpi ulnaris cease instantly proximal to the bases of the metacarpal bones, while those of extensors digitorum, indicis and digiti minimi are typically extended slightly more distally along the metacarpus. Folds of synovial membrane containing a loose plexus of fascial fibres carry blood vessels to the tendons at sure defined factors. Vincula brevia, of which there are two in every finger, are attached to the deep surfaces of the tendons close to to their insertions. There is, thus, one vinculum brevium attaching flexor digitorum profundus to the region of the distal interphalangeal joint, and a extra proximal vinculum deep to flexor digitorum superficialis at the proximal interphalangeal joint. Vincula longa are filiform; usually two are connected to every superficial tendon, one to every deep tendon. The affected sheath thickens and entraps the contained tendons, which turn into constricted on the web site of entrapment and bulge distal to it. This produces a distinct nodule in the palm of the hand and the finger now snaps because the tendon nodule passes by way of the constriction on flexing the finger. The corresponding extensor muscle is insufficiently powerful to extend the affected finger, so the affected person does this passively, accompanied by a painful snap. Treatment regularly requires surgical division of the A1 pulley of the flexor sheath to relieve the stricture. It entails the widespread extensor sheath containing the tendons of abductor pollicis longus and extensor pollicis brevis. There is palpable thickening of the tendon sheath with painful limitation of extension of the thumb. Treatment regularly requires division of the thickened sheath, care being taken to avoid the adjoining superficial radial nerve; division of the sheath produces no functional impairment. A, the lateral side, displaying the anular and cruciate pulleys of the flexor tendon sheath. Details of the anular and cruciate pulleys are proven on the center finger; the extension of the digital arteries and nerves to the end of this finger have been omitted for clarity. These usually cross in a distal course from center finger to index finger, and from ring finger to middle and little fingers. Proximal lacerations to the middle finger extensor tendon may lead to only partial lack of extension because of these tendinous interconnections. Each extensor tendon blends with the extensor enlargement alongside its central axis and is separated from the metacarpophalangeal joint by a small bursa. It receives the conjoined tendons of the interosseous and lumbrical muscular tissues and is almost translucent between its margins and the tendon of extensor digitorum. Transverse fibres (the sagittal bands) pass to the volar plate and transverse metacarpal ligaments, separating the phalangeal attachment of the dorsal interosseous from the relaxation of the muscle, and the palmar interosseous from the lumbrical muscle. The margins of the extensor expansions are thickened on the radial aspect by the tendons of the lumbrical and interosseous muscle tissue, and on the ulnar aspect either by the tendon of an interosseous alone or, in the case of the fifth digit, by abductor digiti minimi. The tendons of the interossei join the extensor growth on the level of the proximal portion of the proximal phalanx, while the tendons of the lumbricals join the extensor mechanism additional distally at the midportion of the proximal phalanx. The extensor mechanism trifurcates into a central slip and two lateral bands just proximal to the proximal interphalangeal joint. The central slip receives a contribution from the tendons of the lumbricals and interossei by way of the lateral bands. Similarly, some fibres from the central area cross to every lateral band, producing a criss-cross arrangement of fibres. The central slip attaches to the bottom of the middle phalanx, while the lateral bands continue distally; they finally fuse together and insert into the distal phalanx. The rigidity within the central slip and the lateral bands varies because the finger moves between flexion and extension and plays a crucial position in coordinating synchronous exercise between the proximal and distal interphalangeal joints. The transverse and oblique retinacular ligaments of Landsmeer join the fibrous flexor sheath to the extensor equipment. The transverse retinacular ligament passes from the A3 pulley of the fibrous flexor sheath on the degree of the proximal interphalangeal joint to the lateral border of the lateral extensor band. The oblique retinacular ligament lies deep to the transverse retinacular ligament. It originates from the lateral aspect of the proximal phalanx and flexor sheath (A2 pulley) and passes volar to the axis of rotation of the proximal interphalangeal joint, but in a dorsal and distal direction, to insert into the terminal extensor tendon. Relations Flexor pollicis brevis lies superficial in the thenar eminence and is distal to abductor pollicis brevis. Testing Flexor pollicis brevis is palpated whilst flexing the metacarpophalangeal joint, with the interphalangeal joint totally prolonged. It arises primarily from the flexor retinaculum, but a quantity of fibres spring from the tubercles of the scaphoid bone and trapezium and from the tendon of abductor pollicis longus. Its medial fibres are connected by a skinny, flat tendon to the radial facet of the base of the proximal phalanx of the thumb, and its lateral fibres join the dorsal digital expansion of the thumb. The muscle may receive accessory slips from the long and brief extensors of the thumb, opponens pollicis, or the styloid strategy of the radius. The thenar muscles include flexor pollicis brevis, abductor pollicis brevis, opponens pollicis and adductor pollicis. The hypothenar muscle tissue embody abductor digiti minimi, flexor digiti minimi brevis and opponens digiti minimi. Relations Abductor pollicis brevis lies proximomedial to flexor pollicis brevis within the superficial part of the thenar eminence. Actions Abductor pollicis brevis draws the thumb ventrally in a airplane at proper angles to the palm of the hand (abduction). The superficial head arises from the distal border of the flexor retinaculum and the distal part of the tubercle of the trapezium, and passes along the radial facet of the tendon of flexor pollicis longus.
Ciprofloxacin 750 mg generic with amex
Major blood vessels enter the gland at the corticomedullary junction and pass inside each lobe bacteria proteus generic 500 mg ciprofloxacin fast delivery, giving off small capillaries to the cortex and larger vessels to the medulla antibiotic skin infection ciprofloxacin 1000 mg generic with amex. Most cortical capillaries loop around at different depths within the cortex and be part of venules on the corticomedullary junction; some continue by way of the cortex and join bigger venules operating in the capsule that depart the thymus. Sheaths of thymic epithelial cells of the blood�thymus barrier lie between the slim perivascular space of the smaller cortical capillaries and cortical thymocytes (Henry et al 1992). Congenital anomalies of the thymus Thymic modifications during postnatal life At birth, the thymus is most frequently bilobar and is 4�6 cm lengthy, 2. The bulkiest a half of the gland at this age is instantly above the base of the heart where it covers the phrenic nerves laterally; the safety of those nerves is mandatory throughout paediatric cardiac surgery procedures. The left lobe is longer and thicker than the right lobe in full-term neonates (Varga et al 2011); throughout childhood, the thymus narrows and lengthens, and the cervical portion becomes much less noticeable. Imaging studies of the thorax in normal children reveal that the proper lobe of the thymus sometimes measures 9 mm in thickness and the left 11 mm. Undescended thymus, accessory thymic our bodies and rare cysts of the third branchial pouch are normally of no scientific significance in isolation. In young children, a large regular thymus may press on the trachea, inflicting assaults of ventilatory stridor. This condition must be differentiated from different congenital circumstances such as vascular rings and slings that require surgical correction. Studies of thymic mass after sudden dying have recorded a wide variation in any respect ages, but the basic pattern is that, after increasing within the first year of life, the imply mass remains fairly constant at 20 g till the sixth decade, when a reduction happens. At start, individual adipocytes are present in connective tissue septa, and elevated numbers are found inside the cortex in the second and third many years. Fatty infiltration is usually complete by the fourth decade, when only the medulla and small patches of related cortex are spared. In youngsters, the gland is more pyramidal in form and firmer than in later life, when the quantity of lymphoid tissue is greatly reduced. With age, it turns into thinner, greyer and more and more infiltrated by yellow adipose tissue. Each of the two lobes is partially divided by the ingrowth of shallow septa, in order that, superficially, the gland seems lobulated. The older thymus may be distinguished from the surrounding mediastinal fats only by the presence of its capsule. However, even greatly atrophied glands usually comprise perivascular areas of persistent lymphoid tissue. Thymocyte manufacturing and differentiation persist throughout life, and thymic T cells continue to populate peripheral lymphoid tissue, blood and lymph. By the onset of puberty, when the main lymphoid tissues are fully developed, thymectomy is less debilitating, however efficient responses to novel antigens are reduced. Thymectomy is usually carried out for myasthenia gravis, usually after referral from a neurologist. The most helpful effects of thymectomy are seen in myasthenic females who current with systemic muscular weak spot; controversial operative teams include the aged and people with isolated ocular symptoms. Generally vertical in its course, the oesophagus usually shows two shallow curves. Starting within the median airplane, it inclines to the left as far as the foundation of the neck, steadily returns to the median aircraft close to the fifth thoracic vertebra, then deviates leftwards again at the seventh thoracic vertebra before piercing the diaphragm. The oesophagus also deviates sagittally because it follows the cervicothoracic vertebral lordosis. In youngsters, the length of the oesophagus correlates greatest with top (Yang et al 2005). The cervical strategy entails a decrease transverse incision that includes the sternal heads of each sternocleidomastoids, allowing an improved access to the substernal airplane. Sternothyroid and sternohyoid are separated and the superior poles of the thymus are identified immediately underneath these muscles. A safe pre-thymic aircraft is created by blunt dissection simply posterior to the sternum, facilitating subsequent mobilization of the gland. The mediastinal nice vessels and the thymic vessels should be rigorously recognized. The thymic veins are selectively ligated and divided, especially these draining instantly into the superior vena cava or the left brachiocephalic vein. The smaller arterial branches from the internal thoracic arteries are usually handled utilizing electrocautery, care being taken to avoid injury to the phrenic nerves (patients are usually not given a paralytic agent during anaesthesia, in order for the phrenic nerves to be identified intraoperatively). The thymus generally remains completely encapsulated and is separated without issue from the pericardium (occasionally, adhesions necessitate a limited pericardiectomy). Further inferiorly, a mild push on the good vessels allows direct visualization into the aortopulmonary window for full elimination of the thymus in this neighborhood. In most cases, the thymus gland is eliminated fully with both upper and lower poles intact. Careful inspection of the remaining tissue within the mediastinum is carried out to identify any attainable anatomical anomalies that may result in retained thymic tissue after the operation. The most common anomaly is the unanticipated location of the higher poles of the thymus behind the left brachiocephalic vein. The aortopulmonary window can be a common location for thymic tissue and this area is typically troublesome to expose with a transcervical strategy. Any suspicious foci of fat in the mediastinum are removed, and, if needed, sent for frozen part to ascertain whether or not they include thymic tissue. Thymic tumours could compress the trachea, oesophagus and enormous veins within the neck, inflicting hoarseness, cough, dysphagia and venous engorgement of the pinnacle and neck. Many affected sufferers also have myasthenia gravis and other autoimmune situations. Myasthenia gravis, a chronic autoimmune disease of adults, presents as a diminution in energy of repetitive contraction in certain voluntary muscle tissue. Although there may be a couple of situation with these signs, myasthenia gravis is essentially an autoimmune disease by which acetylcholine receptor proteins of neuromuscular junctions are attacked by autoantibodies. Muscles commonly concerned are levator palpebrae superioris, leading to ptosis, and the extraocular muscles, resulting in diplopia. Other muscular tissues in the face, jaws, neck and limbs may be involved, and in severe circumstances, the ventilatory muscular tissues are compromised. Posteriorly are the vertebral column, longus colli and the prevertebral layer of deep cervical fascia. Laterally, on all sides, are the widespread carotid arteries and the posterior a half of the thyroid gland. On the proper of the oesophagus, simply above the diaphragm, a small, serous infracardiac bursa may occur, representing the detached apex of the right pneumatoenteric recess.
250 mg ciprofloxacin purchase with amex
The small anterior intercostal veins are tributaries of the internal thoracic and musculophrenic veins; the inter nal thoracic veins drain into the appropriate brachiocephalic vein antibiotic resistance of pseudomonas aeruginosa 500 mg ciprofloxacin with visa. The posterior intercostal veins drain backwards infection elite cme purchase 500 mg ciprofloxacin with visa, and most drain directly or indirectly into the azygos vein on the proper and the hemiazygos or hemiazygos veins on the left. The azygos veins exhibit great variation in their origin, course, tributaries, anastomoses and termination. Intercostal nerves are dis tributed primarily to the thoracic and stomach walls. The larger part of the primary thoracic ventral ramus passes into the brachial plexus, along with a variable proportion of the second. The next four ventral provide only the thoracic wall, and the lower 5 provide each thoracic and stomach partitions. Communicating branches link the inter costal nerves posteriorly in the intercostal spaces, and the decrease five nerves communicate freely in the belly wall. The supraclavicular branches of C4 from the cervical plexus inner vate the skin over the clavicle and may talk with the anterior cutaneous branches of the second thoracic ventral ramus (p. Lymph vessels from deeper tissues of the thoracic partitions drain primarily to the parasternal, intercostal and diaphragmatic lymphatic nodes. The upper eleven lie between the ribs (intercostal nerves), and the twelfth lies below the last rib (subcostal nerve). Preganglionic sympathetic axons originate from neurones in the lateral grey column of the spinal twine from T1 to L2, and depart the spinal cord with the corresponding ventral roots as white rami communicantes. Some enter the sympathetic trunk, where they both synapse in their segmental ganglion, or ascend or descend in the trunk to synapse in cervical or lumbar ganglia. Axons destined for the cervical ganglia are derived from preganglionic neurones in T1. In grownup males, the nipple is normally sited both within the fourth intercostal area or over the fifth rib within the midclavicular line, roughly 20 cm from the sternal notch and midclavicular point (Beckenstein et al 1996). Vagusnervesinthethorax Preganglionic parasympathetic fibres arise from neuronal cell bodies in the dorsal motor nucleus of the vagus in the medulla. Those destined for the thoracic viscera travel in the pulmonary, cardiac and oesopha geal branches of the vagus and synapse in minute ganglia in the visceral partitions. Axons travelling in cardiac branches join the cardiac plexuses and synapse in ganglia distributed over each atria; when stimulated, they gradual the cardiac cycle (Ch. The sternum may be felt all through its size within the midline, though laterally it might be covered by pectoralis major. The jugular (supraster nal) notch is palpable within the midline on the superior sternal border and usually lies on the degree of the junction between the second and third thoracic vertebrae. The cartilaginous rings of the trachea are palpable instantly superior to the notch, using a posteriorly directed finger. The manubriosternal angle is more pronounced within the male than in the feminine, and is palpable on the junction of the manubrium with the sternal physique. It serves as a useful landmark as a result of it indicates the extent of the sternal aircraft and the medial ends of the second costal cartilages, and so presents an correct level at which to start counting ribs. In the vast majority of adults, the sternal angle is situated between the fourth tho racic vertebra and the upper half of the fifth thoracic vertebra, with a spread from the lower half of the second thoracic vertebra to the lower half of the sixth thoracic vertebra, a linear distance of about 8 cm; the airplane lies at a barely higher vertebral level in girls. The xiphisternal joint and xiphoid course of are palpable on the inferior end of the sternum; the joint normally lies on the stage of the ninth thoracic vertebra. Posteriorly, the free ends of the eleventh and twelfth ribs could additionally be Autonomicplexusesinthethorax Cardiac plexus the cardiac plexus has a superficial part inferior to the aortic arch, mendacity between it and the pulmonary trunk, and a deep half between the aortic arch and tracheal bifurcation (Ch. The superficial half is fashioned by the cardiac department of the left superior cervical sympathetic ganglion and the decrease of the two cervical cardiac branches of the left vagus. The deep part is shaped by the cardiac branches of the cervical and upper thoracic sympathetic ganglia and of the vagus and recurrent laryngeal nerves. Branches from the cardiac plexuses also kind the left and proper coronary and atrial plexuses. Pulmonaryplexus the pulmonary plexuses are anterior and poste rior to the other buildings on the hila of the lungs (Ch. They are formed by cardiac branches from the second to fifth (or sixth) thoracic sympathetic ganglia and from the vagus and cervical sympathetic cardiac nerves. Vagal fibres both move via the plexus or are given off immediately by the vagus within the thorax. All fibres relay within the oesophageal wall and are motor to the graceful muscle within the lower oesophagus and secretomotor to mucous glands within the oesophageal mucosa. Vasomotor sympathetic fibres come up from the upper six thoracic spinal twine segments. Those from the upper segments synapse in cervical ganglia; postganglionic axons innervate the vessels of the cervical and higher thoracic oesophagus. Fibres from the lower segments pass on to the oesophageal plexus or to the coeliac ganglion, where they synapse; postganglionic axons innervate the vessels of the distal oesophagus. The accuracy of some older descrip tions of clinically necessary surface landmarks, primarily based on cadaveric or radiographic studies, has been questioned just lately (Hale et al 2010). The tail of the breast extends in direction of the axilla alongside the infero lateral border of pectoralis major (Ch. Key: 1, proper acromioclavicular joint; 2, clavicle and mid-clavicular line (dashed black); three, apex of right lung, located posterior to the medial third of the clavicle; four, sternal notch of manubrium sterni: the trachea could additionally be located here by posterior palpation; 5, sternoclavicular joint: marks the junction of the internal jugular and subclavian veins to type the brachiocephalic vein; 6, zone of formation of the superior vena cava: from first intercostal space to second costal cartilage degree (78% of subjects, white zone); 7, sternal angle: marks the extent of the sternal plane and the second costal cartilage; eight, pectoralis major and the anterior axillary fold; 9, horizontal fissure; 10, proper oblique fissure; eleven, decrease anterior border of the right lung: typically, either the sixth intercostal area or the seventh rib in the mid-clavicular line; 12, decrease anterior border of the left lung: typically, both at the fifth rib or fifth intercostal house within the mid-clavicular line; 13, xiphisternum; 14, costal margin; 15, tenth costal cartilage, forming the lower part of the costal margin. The levels of the spinous processes of the third, ninth and twelfth thoracic vertebrae and the first lumbar vertebra are indicated within the midline. Key: 1, border of the left lung; 2, oblique fissure: passes anteroinferiorly from the spinous process of the third thoracic vertebra to cross the fifth rib within the midaxillary line. The higher lobe sits superiorly and the lower lobe inferiorly; three, decrease border of the lung: this is often situated at stage of the twelfth thoracic vertebra however may be lower, on the level of the first lumbar vertebra, adjoining to the vertebral column at finish tidal inspiration. Dashed blue traces indicate the vary of ranges for the decrease border of the lung (ninth thoracic vertebra to first lumbar vertebra); 4, twelfth rib: could be traced superomedially to aid identification of the spinous means of the twelfth thoracic vertebra. Posteriorly, the spinous processes of the thoracic vertebrae are palpable; the spinous process of the first thoracic vertebra sits under that of the seventh cervical vertebra (vertebra prominens) and is often extra prominent. The angles of the ribs are palpable a number of centimetres lateral to the spinous processes of the vertebrae. Key: 1, internal jugular vein; 2, subclavian vein; three, formation of the brachiocephalic vein posterior to the sternoclavicular joints; four, formation of the superior vena cava, posterior to the best second costal cartilage or first intercostal area; 5, manubriosternal joint, 6, concavity of the aortic arch, sometimes sitting inferior to the sternal plane, level with the higher half of the fifth thoracic vertebra; 7, azygos vein coming into the superior vena cava: typically, it sits inferior to the sternal airplane, degree with the lower half of the fifth thoracic vertebra; 8, tracheal bifurcation: usually, it sits inferior to the sternal plane, stage with the higher half of the sixth thoracic vertebra; 9, bifurcation of the pulmonary trunk, stage with the higher half of the sixth thoracic vertebra, roughly three cm inferior to the sternal angle. The sternal plane is conventionally described as lying over the tracheal bifurcation, the concavity of the aortic arch and the point where the azygos vein enters the superior vena cava. Not reported T6 upper (28%) (T4/5 to T7/8) Measurements relative to the sternal aircraft are shown as + (superior to the plane) and - (inferior to the plane). They may be modified by age, intercourse, stature, ventilation, the posi tion of the diaphragm and posture (Macklin 1925).